What We Know About Value-Based Care Under MACRA, MIPS, APMs
MACRA and its many provisions in Section 101 go into effect in 2019. Here's what we know so far.

Source: Thinkstock
- The Medicare Access and CHIP Reauthorization Act of 2015 has many parts tied to Medicare and other federal health plan beneficiaries, but first and foremost it is a bill that brings an end to the sustainable growth rate and a beginning to new incentive programs for providers working in a value-based care ecosystem.*
*NB. HHS recently announced the publishing of the proposed rule for MACRA implementation, which changes many of the provisions described herein.
Given all the debate over a lack of alignment of quality reporting programs at the Centers for Medicare & Medicaid Services (CMS), these new value-based care incentive programs are drawing considerable interest. With the final rule for Merit-Based Incentive Payment System (MIPS) and Alternative Payment Models (APMs) currently under review by the Office of Management and Budget, that interest is compounded.
While the particulars of these programs are not yet known, details about them do exist.
Source: CMS
Getting to Know Section 101
The first section of MACRA lays out the main provisions of the bill, which are twofold.
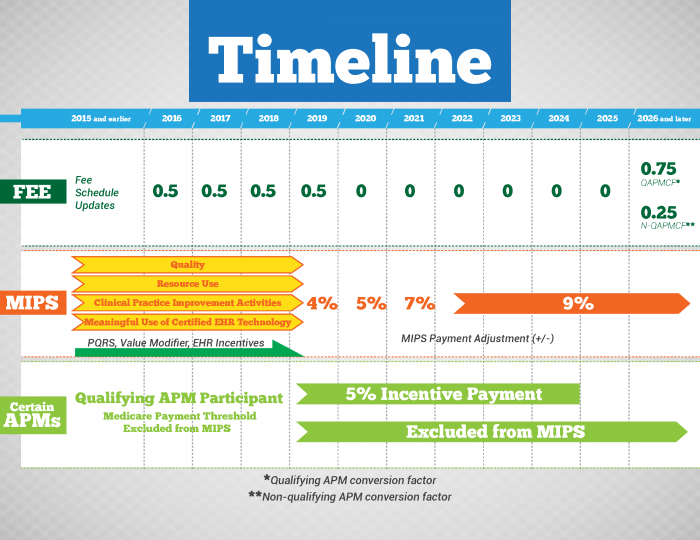
First, MACRA repeals the SGR and replaces it with a consistent fee schedule over the next decade that takes into account provider participation in value-based care programs. Beginning in 2016 and extending through 2019, fee updates are 0.5 percent annually.
Beginning in 2026, these rates take into conversion factors for qualifying and non-qualifying alternative payment model participants — 0.75 percent for the former and 0.25 percent for the latter.
The SGR repeal also requires the Medicare Payment Advisory Commission (MedPAC) to submit reports to Congress as early as July 1, 2017, on provider utilization and expenditures and all providers.
Second, MACRA creates MIPS and APMs. The former brings extant quality reporting programs under one roof. The affected programs are the EHR Incentive Programs, Physician Quality Reporting System (PQRS), and Value-based Payment Modifier (VPM). Under MACRA, these programs do not end but instead become part of a formula for scoring the performance of eligible professionals in value-based care settings.
Details on Merit-Based Incentive Payment System
Professinals eligible for MIPS
Source: Massachusetts eHealth InstituteMACRA tasks the Department of Health & Human Services with three activities relative to MIPS. The first and second are to develop the methodology for assessing EP performance and produce a composite performance score. The third and final is to use this score to apply payment adjustments, both positive and negative.
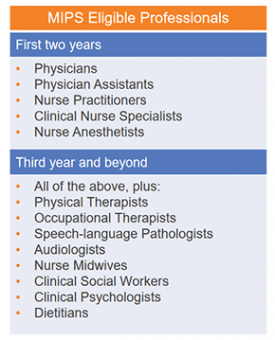
MIPS eligibility is similar to the quality reporting programs the system has subsumed. For the first two years of the provide, eligibility applies to Medicare physicians, physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists. In year three, the HHS has the discretion to include other EPs.
Those excluded from MIPS participation are providers working as part of an APM or partial qualifying APM participants — "an eligible professional for whom the Secretary determines the minimum payment percentage" but whom the Secretary considers to have satisfied the conditions of a qualifying APM participant.
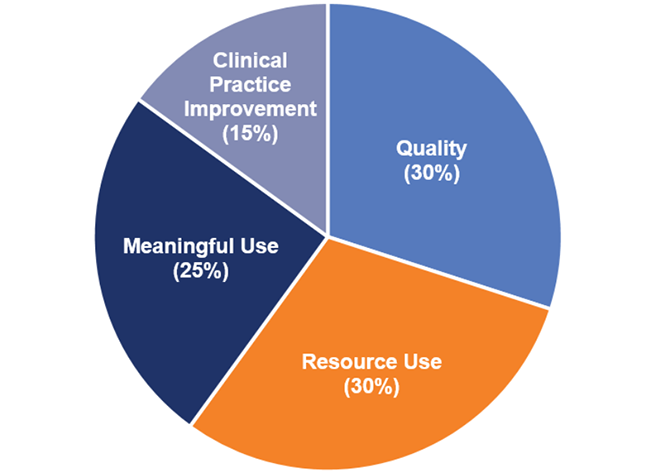
Under MIPS, CMS will use four performance categories to assess providers with positive, negative, or neutral payment adjustments — quality, resource use, clinical practice improvement activities, and meaningful use.
The quality and resource use categories each account for 30 percent of the composite performance score, followed by meaningful use at 25 percent and clinical practice improvement activities at 15 percent.
The bill does contain a provision allowing HHS to modify the percentage assigned to meaningful use in the event that EHR adoption exceeds 75 percent of eligible providers.
So in short, here's the math:
Source: Massachusetts eHealth Institute
As for the individual measures used by each of the four programs contributing to a provider's composite score, fewer specifics are available at this time.
For the quality category, HHS has the annual responsibility of producing a final list of quality measures for MIPS providers to choose from. The quality measures will be culled from industry feedback, peer reviewed, and published each November.
As CMS noted in a request for information on MACRA, the federal agency will apply lessons learned from PQRS and VPM to "help shape processes and policies for this performance category." CMS is considering multiple mechanisms for reporting quality performance (e.g., individually, as a group) as well as the means of reporting (e.g., via certified EHR technology).
For resource use, CMS is entertaining using a methodology based on the VPM:
- Total per capita costs for all attributed beneficiaries measure;
- Total per capita costs for beneficiaries with specific conditions (diabetes, coronary artery disease, chronic obstructive pulmonary disease, and heart failure)
- Medicare spending per beneficiary (MSPB) measure
For clinical practice improvement activities, the MACRA legislation is prescriptive as to the subcategories necessary for inclusion: expanded practice access, population health management, care coordination, beneficiary engagement, patient safety and practice assessment, and APM participation. Additionally, it calls on CMS to give special consideration to providers in rural and underserved geographies.
The meaningful use category contains no other details than a provider's need to demonstrate meaningful use during a specific performance period.
While the specifics of MIPS requirements are still taking shape, the financial rewards or penalties are more clear cut. MIPS EPs scoring at or above the performance threshold will receive a zero or positive payment adjustments; those scoring below, a negative payment adjustment.
In 2019, the adjustment percentage is set at 4 percent. In 2020 and 2021, it is set at 5 percent and 7 percent, respectively. For 2022 and beyond, the figure is 7 percent. Exceptional performance opens MIPS EPs up to an increase adjustment percentage to be determined by HHS.
The formula shakes out as follows:
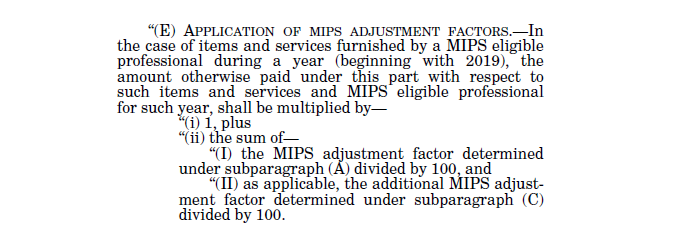
Source: CMS
As specified in the legislation, CMS will gauge performance for each individual year and not include adjustment factors from previous years.
Details on Alternative Payment Models
For those providers looking to forgo MIPS participation, MACRA provides a second path toward value-based care — alternative payment models (APMs). These programs include the Medicare Shared Savings Program and the like
No later than Nov. 1, 2016, HHS must issue a final rule establishing criteria for physician-focused payment models, otherwise known as APMs, based on feedback from industry stakeholders as well as MedPAC and others.
APM participants not only receive payment for delivering professional services but also make themselves eligible for an incentive payment equal to five percent " of the estimated aggregate payment amounts for such covered professional services under this part for the preceding year." Payments will come in the form of lump sum annually and "as soon as practicable."
Between 2019 and 2020, qualifying APM participants are EPs that furnish 25 percent or more of their professional services as part of an eligible alternative payment entity. Between 2012 and 2022, that percentage rises to 50 percent. In 2023, the figure rises to 75 percent.
Qualifying APM participants must satisfy requirements similar to those required of MIPS participants. First, eligible alternative payment entities must require participants to use certified EHR technology, base their provision of professional services on quality measures "comparable to measures under the performance category," and be engaged in risk-based arrangements.
The legislation leaves open the possibility for HHS to determine an EP's status as a qualifying APM participant based on patient counts.
A crucial component of MACRA relative to APMs is the creation of the Physician-focused Payment Model Technical Advisory Committee, which is responsible for advising HHS on its eponymous PFPMs. According to CMS, the latter represent an avenue for other EPs to qualify for and receive incentives.
"PFPMs are not required by the MACRA to meet the criteria to be considered APMs," the federal agency stated in its MACRA RFI. "However, we are interested in encouraging model proposals from stakeholders that will provide EPs the opportunity to become QPs and receive incentive payments."
Technical Assistant for Certain Providers
In the MACRA legislation, Congress has recognized the challenge of value-based care for providers in certain geographies. Under MACRA, HHS " is required to enter into contracts or agreements with entities such as quality improvement organizations, regional extension centers and regional health collaboratives beginning in Fiscal Year 2016 to offer guidance and assistance to MIPS EPs in practices of 15 or fewer professionals."
The bill gives priority to small practices located in rural areas, health professional shortage areas (HPSAs), and medically underserved areas, and practices with low composite scores. Additionally, the assistance will focus on provider performance under MIPS as well as support in working on APMs.
MACRA Impact on Health IT
While the provisions of Section 101 under MACRA do not become effective until 2019, subject matter experts have already highlighted the need for health IT improvements to assist providers in their transition to value-based care.
According to a recent Impact Advisors report, EHR optimization is one such area for improvement.
"With providers having more and more to do during an office visit, including everything from preventive care, chronic disease management, capturing quality data, filling care gaps and adequately documenting for both clinical care and billing purposes, it is imperative to the success of healthcare organizations to make provider use of EHRs efficient," states the report.
"Most organizations have done little since EHR implementation to actually improve provider efficiency in the system," it continues, "but going forward there will need to be considerable focus on specialty-specific build, minimizing clicks, making quality measure documentation streamlined and intuitive, and presenting providers with feedback in the form of performance dashboards."
Until the final rule for MACRA, MIPS, and APMs hits the Federal Register, healthcare organizations and providers have little concrete information to go on as to preparing their clinicians for the federal government's implementation of value-based care.
