2 Medicare Alternative Payment Models Demanding Future Focus
Healthcare providers are coming closer to reaching their alternative payment model goals. But they will fall behind without timely, reliable data and better coordinated care efforts.

- Medicare alternative payment models have the ability to make affordable, high quality care a reality.

But providers still demand greater levels of care coordination and cleaner streamlining of clinical data to achieve value-based reimbursement success.
Sylvia M. Burwell, Secretary of the Department of Health and Human Services (HHS) announced in early 2015 an expedited transition towards alternative payment models.
According to HHS’s proposed timeline, 30 percent of payments are planned to be value-based by the end of this year.
HHS said this number will hopefully hit 50 percent by the end of 2018.
The Centers for Medicare & Medicaid Services (CMS) said its timeline is indeed doable.
“These are measurable goals to move the Medicare program and our healthcare system at large toward paying providers based on quality, rather than quantity, of care,” CMS claimed.
This important news is still making an impact on the industry as the fee-for service payment realm diminishes with time.
Alternative payment models need to be a primary focus for the industry moving forward to ensure smooth claims reimbursement and the ongoing delivery of top-notch care.
Here is a deeper look at how two of these specific alternative payment models – bundled payments and accountable care organizations (ACOs) – are progressing.
Diving into the fundamentals of bundled payment models
Sharing is caring when it comes to bundled payments.
Under this prospective payment model, a single payment involving a variety of services is shared among various providers across different settings.
The primary objective of the bundled payment model is to foster more dynamic relationships and productive partnerships by making the payment process a tad less isolated.
CMS confirmed bundled payments allow for greater provider adaptability and flexibility in deciding how payments are allocated across participating providers.
But the bundled payment design still demands a bit of tweaking in regard to care coordination efforts, said the American Hospital Association (AHA) last April.
Bundled payment arrangements “present many challenges, as providers will face substantial risk if they do not have tools available to understand and select the post-acute and other services that will achieve the best outcome for a given patient,” the AHA stated.
”Our members strive to provide the right care in the right setting, but a lack of care coordination in the fee-for-service system produces significant variation in how patients receive post-acute care,” the organization added.
The AHA additionally confirmed support for the testing of new models on a small scale and “using the lessons learned to develop proposals before considering widespread adoption and implementation.”
Nearly two months later, the Workgroup for Electronic Data Interchange (WEDI) announced the formation of a Bundled Payments Taskforce.
Its goal was to examine how bundled payment initiatives were unfolding, especially in connection with the value-based reimbursement transition.
WEDI was particularly interested in streamlining the exchange of clinical and administrative data among payment models.
The organization also remained focused on effectively utilizing technology to ensure payment-related data was being seamlessly relayed between parties.
As these and other bundled payment initiatives advance, the Medicare payment shift continues onwards.
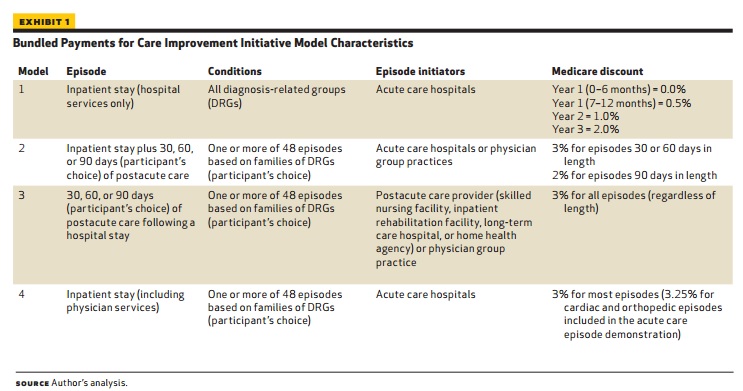
Particularly worthy of note is that CMS’s Bundled Payments for Care Improvement Initiative (BPCI) began in January of 2013.
Under this initiative via the Affordable Care Act (ACA), CMS worked with a variety of organizations to determine how and why bundled payment models lower Medicare costs and improve patient care.
CMS confirmed that as of last month, its BPCI initiative had over 1,500 participants, including 409 acute care hospitals, 700 skilled nursing facilities, 288 physician group practices, and 100 home health agencies.
But hospitals are apparently struggling with their BPCI endeavors, especially in regard to maintaining accurate, up-to-date risk-adjustment pricing data.
“If healthcare providers have timely, reliable data, the Bundled Payments initiative presents a great opportunity to reduce costs, decrease readmissions, and enhance patient care,” Andre Blom, Director of Rehabilitation at the Illinois Bone & Joint Institute said.
“But if the data isn’t trustworthy, the benefits of the program will elude them,” he said. “They will need to fix the infrastructure that has failed to provide accurate, actionable information.”
“If hospital administrators are working with retrospective information, if their data is two years old, it’s irrelevant today,” he added.
Investing on the front-end with merely unguaranteed return on investment on the back-end is not necessarily appealing to the medical community at large.
Blom advised hospital executives to evaluate the overall scope of their health system and identify blind spots. Additionally, noting what elements may simply be beyond their control is imperative for success, he stated.
“Healthcare is changing into a retail environment. With high deductible plans, healthcare providers are realizing the need to view patients as collaborators in value-based care initiatives and redesign,” he explained.
Executives are able to track their risk bearing entities with real-time, accurate data at their fingertips, he said.
And care coordination technology solutions are helping them efficiently connect the dots between various patient episodes across an entire acute and post-acute network, he stated.
Investing a given amount of money is less painful if the back-end amount can be estimated accordingly early on, he added.
Many across the industry believe bundled payments simply represent a better way to practice medicine, he claimed.
“The paradigm shift to value-based care is forcing people to start talking to one another about what’s going on, which is new,” he said. “They are communicating inside and outside of their system because they recognize they need to be able to take care of the whole patient.”
Accountable care organizations are about quality measures
Under the Medicare Shared Savings Program for ACOs, providers who willingly coordinate patient care and who meet around 30 different quality measures – including patient experience, patient safety, and at-risk populations – can experience increased savings, CMS confirmed.
“ACOs which elect to become accountable for shared losses have the opportunity to share in greater savings,” said CMS.
“The higher the quality of care providers deliver, the more shared savings their Accountable Care Organization may earn, provided they also lower growth in health care expenditures,” CMS added.
A great deal of positive ACO news has been swirling across the healthcare industry in recent months.
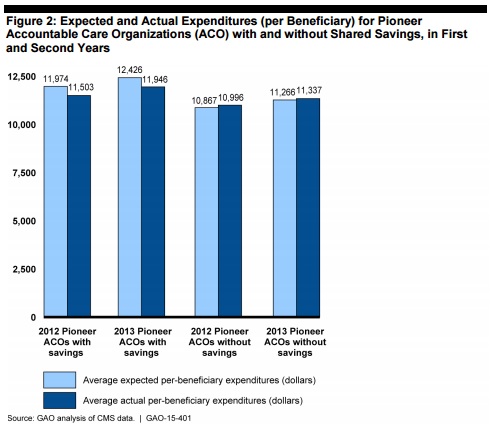
ACOs reportedly have been assuming high levels of risk while generating over $411 million in net program savings within a one-year period, CMS reported.
“In the third performance year, Pioneer ACOs showed improvements in 28 of 33 quality measures and experienced average improvements of 3.6% across all quality measures,” CMS said.
“Shared Savings Program ACOs that reported quality measures in 2013 and 2014 improved on 27 of 33 quality measures,” the organization stated.
And Pioneer ACOs alone have generated over $380 million in Medicare savings, according to HHS.
“The Pioneer ACO Model has demonstrated that patients can get high quality and coordinated care at the right time, and we can generate savings for Medicare and the health care system at large,” stated Burwell last May.
But there is still a steep educational learning curve when it comes to relatively new ACOs.
ACOs may need to adopt tighter standards and more openly embrace technological opportunities to stay afloat.
“The lower cost connection is that hospitals are going do an asset allocation of their revenue stream,” explained Dutch Dwight, Medullan’s Vice President of Business Development.
Successful ACOs must drive more standards adoption, he claimed.
“Across the healthcare industry there have yet to be transformational solutions to enable a dramatic reduction in cost per claim. Many ideas have been bantered about, but none have been combined in a fundamental way,” Dwight added.
The Pioneer Program was a vital learning experience for the greater industry.
“The Pioneer Program was sort of a big experiment in value-based or risk-based contracting,” Johnathan Niloff, MD, McKesson’s Chief Medical Officer, said.
“CMS and CMMI view this program as a success because of its effectiveness in improving quality metrics and in reducing total cost of care,” he said.
“A number of the parameters of the original Pioneer Program did not create the optimal environment for an organization to be able to manage an at-risk population from a perspective of coordination of care across the continuum,” Niloff stated.
“The organization needs to come to terms with internal conflicts and unify around a strategy to move forward and successfully transition. They have to align their objectives and incentives among all their constituents,” he added.
Niloff advised implementing a coordinated care model around a primary care medical home model to help coordinate care across a wider continuum.
“You need a methodology to identify high-risk patients and then a care management program to manage the care of those high-risk patients,” he said.
“You need analytics to understand the key drivers of your total cost of care and to be able to manage those drivers,” Niloff added.
“In a value-based or ACO world, what historically a CFO might have thought of as a revenue center becomes a cost center in a total-cost-of-care model,” he relayed.
Key drivers that are helping providers align their efforts with CMS’s alternative payment model timeline, he said, include the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and the Merit-Based Incentive Payment System (MIPS).
“The passage of [MACRA] supports the ongoing transformation of healthcare delivery by furthering the development of new Medicare payment and delivery models for physicians and other clinicians,” said CMS.
“CMS is committed to reducing provider burden through the use of measures aligned across federal and private-payer quality reporting programs,” the organization stated.
“We stress harmonization of data elements and specifications among measure developers, whose cooperation and sharing are essential to creating aligned measures.”
Image Credits: [Health Affairs] (Image 1)
Image Credits: [United States Government Accountability Office] (Image 2)
