3 Key Steps to Continue ICD-10 Implementation Progress
The ability to measure outcomes is key when it comes to ICD-10 implementation as it can show a provider how far the organization has come and address ways to maintain momentum.

- Now that the ICD-10 implementation has been deemed a relative success throughout the healthcare industry, the Centers for Medicare & Medicaid Services (CMS) are focused on continuing the progress related to the ICD-10 implementation. CMS released a new infographic meant to assist healthcare providers in remaining accurate in their ICD-10 claims processing.

Creating baseline for key performance indicators
The ability to track and measure outcomes is key when it comes to ICD-10 implementation as it can show a provider how far the organization has come and address ways to maintain the momentum. First, CMS recommends providers to create a baseline for key performance indicators, which essentially means developing a point of reference for each performance indicator one is looking to measure.
CMS also provided a new resource on key performance indicators to assist providers in gaining a greater understanding of their achievements in ICD-10 implementation. Smaller medical practices may not have had as much opportunity to track key performance indicators and this worksheet includes a list of these indicators that may be helpful for providers.
One step to take with regard to key performance indicators is to create another baseline with current data, CMS explains. Medical billing and coding staff as well as clearinghouses and vendors could assist in the process as well.
Addressing feedback on the ICD-10 implementation
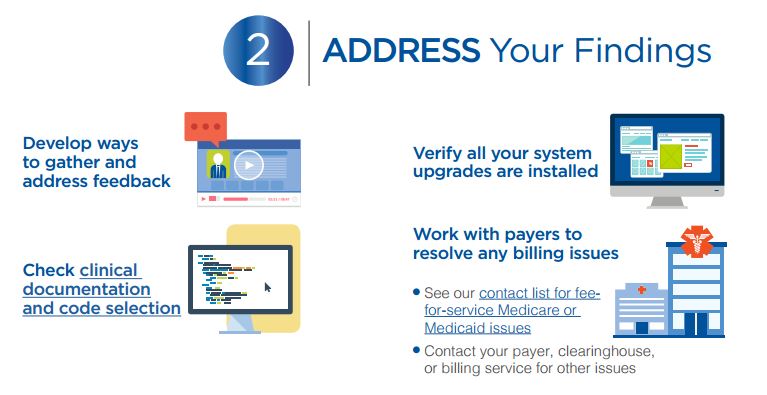
The second part of the infographic explains that healthcare providers should “develop ways to gather and address feedback.” This means getting feedback from staff and those working within the healthcare organization who use ICD-10 coding on a daily basis. Asking staff to clarify whether there are certain workflows that may be impeded by ICD-10 code selection is useful as well as determining areas for improvement.
Additionally, it is always encouraged to clarify and recheck ICD-10 code selection and medical documentation practices. If issues come up, it may be important to conduct more staff training and provide educational resources on ICD-10 best practices and ID-10 coding concepts. Without sufficient staff training, the transition to the new coding system could cause claim denials and delays in payment.
It is important to address whether documentation differences are due to payer requirements, templates set up by the vendor, or mainly due to the providers. Every organization will need a specific process when selecting ICD-10 codes for each medical record.
Upgrading IT systems to align with ICD-10 coding
It is also useful to check whether system upgrades have been fully installed in updated software products. Providers should verify if there are any technical issues with their IT systems, as these problems could also lead to delays in claims processing and denials.
Most importantly, IT platforms will need to ensure all services billed before October 1, 2015 utilize ICD-9 codes and all services performed after the implementation date should have ICD-10 codes. As always, providers will need to address any medical billing problems with payers including Medicare and Medicaid insurers.
In order to continue on the ICD-10 implementation progress already built, coding tools and IT systems will need to be updated regularly. On October 1, 2016, the annual update for ICD-10 coding will occur.
In November 2015, RevCycleIntelligence.com interviewed Michael Creef, MD, a Virginia-based family physician to find out how healthcare providers were faring with upgrading and implementing electronic health records to align with ICD-10 diagnostic codes.
“Last October, we were not into electronic records,” the family practitioner mentioned. “This changed when it appeared ICD-10 was not only on the horizon but the horizon had arrived.”
“I picked EHR use up very quickly, was pleased with it, and was able to impart it to my colleagues. Consequently, this has decreased the amount of time a patient was spending on paperwork and helped us to be able to get things rolling on a much faster basis,” said Creef.
“Years ago, I said I wasn’t interested in electronic records. Now I’m not only interested in it, I’m teaching them, and I like it,” Creef exclaimed. “You can teach old dogs new tricks, believe me. The oldest member of our group is 83 and even he’s come around to it.”
Creef also explained that not everyone is as interested in sticking to the new coding guidelines, as was evidenced by several lawmakers who proposed pushing back the ICD-10 deadlines or even sticking with the older diagnostic codes for the time being.
“Things have changed. Physicians and other healthcare providers need to understand that they have to get on board with this, like it or not,” he said. “Our staff and patients have been more than willing to work with us in the new advent of ICD-10. They understand exactly what we’ve been going through because we’ve been quite honest with them to let them know about the new coding.”
“The billing company we have is very good at catching whether or not a code is specific enough. Our doctors are very good about putting in code laterality and specificity,” Creef concludes.
CMS also advised medical practices to review ICD-10 General Coding Guidelines while hospitals should keep an eye on the General Coding Guidelines for ICD-10 inpatient procedure coding.
By following these guidelines, healthcare providers should be set to continue their success and progress with the ICD-10 implementation. This will keep the revenue cycle in check and ensure medical claims are reimbursed in a timely manner.
Image Credits: Centers for Medicare & Medicaid Services