Accountable Care Organizations Responsible for Drug Spending
The report found that pharmacists are being underutilized among accountable care organizations since only 57 percent of providers are contracting with pharmacists.

- Accountable care organizations consist of a network in which payers, primary care physicians, and specialists work together to improve the health of a population. To dive deeper into one of the type of specialists seeking to enhance care within an accountable care organization, the Pharmacy Benefit Management Institute released a report detailing pharmacy trends within the ACO setting.

The study looked at more than 100 ACO providers among 6.5 million beneficiaries, according to a press release from the Pharmacy Benefit Management Institute. To provide additional information on drug benefit trends and the ongoing news from the ACO market, the Institute will publish four national industry reports from now on.
“ACOs represent a critical and growing part of the solution to help improve value, quality, and care in our nation’s health care and pharmacy plays an important role in achieving those goals,” Jane Lutz, Executive Director of the Pharmacy Benefit Management Institute, said in a public statement. “Our new ACO report looks specifically at valuable information regarding contract and financial incentive structures, current practices in pharmacy management, and plans for the future.”
The report found that pharmacists are being underutilized among accountable care organizations since only 57 percent of polled providers are contracting with clinical pharmacists. Additionally, most of the respondents regard population health management as a vital part of running a successful accountable care organization.
The results show that 93 percent said managing population health is either “very or extremely important” while 98 percent stated that population health management will be targeted even more in the next three to five years.
One area that poses a problem for interoperability, care coordination, and data sharing is the fact that 59 percent of respondents from accountable care organizations use multiple EHR systems and 23 percent are still using paper-based charts. Not even one out of three respondents stated being on a single electronic medical record platform.
The majority of respondents are also using support tools. When it comes to medication management, the major goals of those polled includes strengthening adherence, drug selection, and cutting down on inappropriate use.
Along with some of these findings, 56 percent of polled providers stated that accountable care organizations will lower the costs associated with prescription drug therapy while 69 percent stated that ACOs will likely improve the “quality of prescription drug therapy.”
One research paper published in the Journal of Managed Care & Specialty Pharmacy delved into whether the contracts of accountable care organizations require these providers to be responsible for prescription drug spending. Additionally, more information was gathered on how accountable care organizations manage the utilization of prescription medication and engage pharmacies.
The costs of prescription drugs relates directly to overall healthcare spending across the industry. Innovative care delivery networks like the accountable care organization or the patient-centered medical home could bring real change to the costs of prescription medication and general healthcare spending.
In the study, out of ACOs working with commercial payers, 77 percent stated that their contracts held them accountable for prescription drug spending. Among Medicare, Medicaid, and commercial contracts, 45 percent stated that at least one had them bear responsibility for prescription drug costs.
The results also showed that half of ACOs had a “formal relationship with a pharmacy.” One-quarter of polled providers had a pharmacy working within the accountable care organization. Additionally, almost one-fifth of ACOs studied in the report employed contracted pharmaceutical services.
The study outlined that ACOs who work more directly with pharmacies tend to have greater experience in payment reform, both private and public contracts, and have access to more provider types.
With regard to overall success in the ACO setting, contracts that include greater responsibility for prescription drug spending and pharmacy networking will bear necessary. The study showed that commercial payers were more likely to include accountability for prescription medication costs among ACOs while Medicare contracts did not include such clauses.
“While Medicare has not included pharmacy spending in its accountable care programs, ACOs with commercial contracts are, for the most part, held responsible for pharmacy spending,” the report published in the Journal of Managed Care & Specialty Pharmacy stated.
“More advanced ACOs—those with more payment reform experience, multiple contracts, and a diversity of providers—are the most likely to include a pharmacy. This finding may indicate that these ACOs understand the importance of ensuring effective and efficient prescribing and adherence to achieving quality and cost goals, or that integrated systems with pharmacy services are more likely to take on the risk of new payment contracts.”
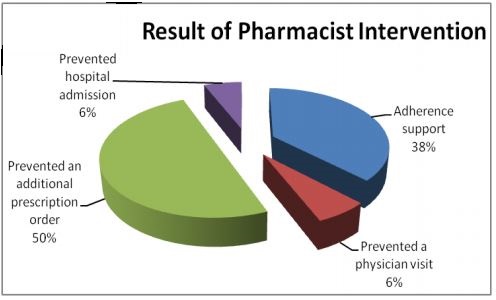
Blue Cross of California also discussed the importance of utilizing pharmaceutical services in adequate levels within an ACO. The graphic below illustrates the patient benefits of pharmacist intervention.
As accountable care organizations gain greater experience, earn shared savings, and develop payment reform protocols, they will move closer to achieving the Triple Aim of improved patient satisfaction, better health outcomes, and lower medical costs.
The accountable care organization could play a significant role in managing medication costs in the coming years by encouraging the use of cost-effective prescription drugs among patients with chronic disease and contracted pharmacies.
Image Credits: Blue Cross of California