Avoidable Hospitalizations Drop 31% for Long-Term Care Patients
Value-based care models contributed to a significant decrease in avoidable hospitalizations among dual-eligible long-term care patients, CMS stated.

Source: Thinkstock
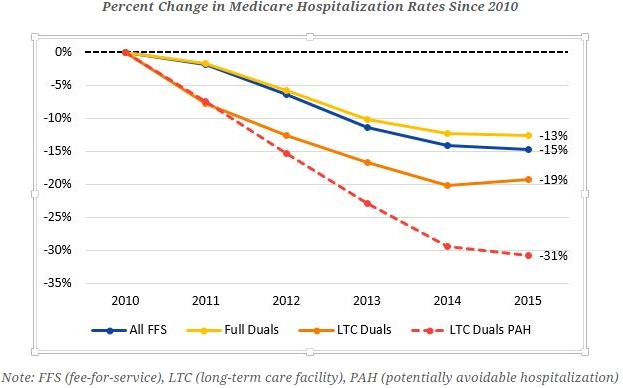
- Avoidable hospitalizations among dual-eligible long-term care facility residents dropped by 31 percent between 2010 and 2015 largely because of value-based care programs, CMS recently stated in an official blog post.
“Family members want to be assured that their loved one will receive the highest quality of care in a healthy environment,” stated the blog post. “And thanks to efforts across the healthcare industry, and with tools from the Affordable Care Act that allow CMS to improve quality and test innovative strategies, these residents are living in safer, healthier environments.”
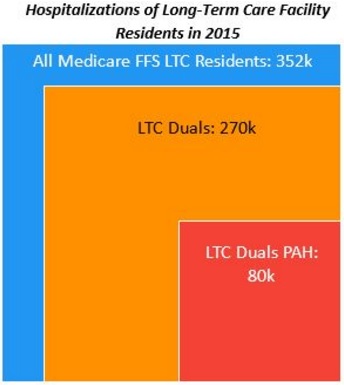
Dual-eligible beneficiaries were the most vulnerable population to hospitalizations among long-term care residents. Medicare fee-for-service beneficiaries in long-term care facilities had 352,000 hospitalizations in 2015. But dual-eligible beneficiaries in the long-term care facilities accounted for 270,000 of the total hospitalizations.
Source: CMS
Furthermore, about one-third of the dual-eligible hospitalizations were caused by six potentially avoidable conditions, including asthma, skin ulcers, bacterial pneumonia, congestive heart failure, dehydration, chronic obstructive pulmonary disease, and urinary tract infections.
While the overall Medicare hospitalization rate for dual-eligible beneficiaries decreased by 13 percent from 2010 to 2015, CMS value-based care initiatives helped dual-eligible long-term care facility residents to experience even less hospitalizations, especially for the six potentially avoidable conditions.
Source: CMS
In 2010, about 227 per 1,000 dual-eligible beneficiaries in long-term care facilities faced a potentially avoidable hospitalization. By 2015, however, the rate plunged to just 157 per 1,000 beneficiaries.
As a result, dual-eligible long-term care facility residents avoided about 133,000 hospitalizations during the five-year period.
CMS attributed decreasing avoidable hospitalization rates to providers who treated older adults and individuals with disabilities. But the federal agency also credited its value-based reimbursement programs.
For example, the CMS Innovation Center and the Medicare-Medicaid Coordination Office launched a value-based care initiative in 2011 to decrease avoidable hospitalizations among nursing facility residents. The program ran across seven states and aimed to prevent the six conditions in dual-eligible residents.
The three-year initiative reduced potentially avoidable readmissions by about 28 percent and saved Medicare over $5 million, CMS reported in January 2016.
Based on initial successes, the federal agency expanded the initiative in six states last year. One program participant in Pennsylvania told RevCycleIntelligence.com in November 2016 that CMS added more value-based incentive payments to the initiative, including care coordination compensation and higher Medicare reimbursement rates for treating residents in the nursing home.
“By adding some of these increased incentives back into the nursing home, we are increasing the quality of care that they can provide, but then it’s also allowing them to be that player that is actively engaged in that beneficiary’s care across the continuum,” said April Kane, Co-Director of the initiative at University of Pittsburgh Medical Center. “They are just as important as our hospital setting and our community setting.”
CMS also mentioned in the blog post that other value-based reimbursement initiatives contributed to lower avoidable hospitalization rates among long-term care facilities. For instance, the federal agency noted that the Hospital Readmissions Reduction Program helped to avoid hospitalizations at long-term care facilities.
Under the value-based reimbursement program, Medicare beneficiaries avoided about 100,000 unnecessary readmissions 2015, CMS reported in September 2016. In total, Medicare beneficiaries avoided about 565,000 readmissions since 2010.
In addition, the federal agency attributed decreasing avoidable hospitalization rates among long-term care facilities to the healthcare industry’s value-based reimbursement transition. Through alternative payment models, such as accountable care organizations and the Bundled Payments for Care Improvement initiatives, healthcare stakeholders worked to improve care quality.
The Agency for Healthcare Research and Quality’s Safety Program for Long-Term Care also decreased catheter-associated urinary tract infections. As a result, long-term care providers in the program prevented one of the potentially avoidable conditions that result in hospitalization.
“This success shows that a sustained commitment to smarter spending across the entire healthcare system can yield dramatic results and improve the lives of vulnerable Americans,” stated the blog post.
