Bundled Payments, Clinical Pathways Drive Cancer Care Savings
Oncology value-based reimbursement models used bundled payments and clinical pathways to reduce cancer care costs, but researchers suggest incentives for innovation.

Source: Thinkstock
- Early adopters of value-based reimbursement models for oncology realized significant cancer care savings through bundled payments and clinical pathways, a recent Evidence-Based Oncology study revealed. But the financial incentives for the models may have hindered providers from prescribing new treatments.
“With rapid advances in diagnostics, precision medicine, and immunotherapy, how can a standardized payment model be defined that leaves room for innovation,” researchers from Deloitte Center for Health Solutions wrote. “Our research revealed that many organizations are experimenting with value- based payment models that aim to balance the competing goals of controlling costs and allowing access to advances in treatment.”
Using interviews with 18 individuals from provider groups, clinical pathway developers, and health plans, researchers found that four oncology-specific value-based reimbursement models generated early signs of success. The four models used by the stakeholders were:
• Financial incentives for adhering to clinical pathways
• Patient-centered medical homes
READ MORE: Cancer Costs Don’t Rise Faster than Other Healthcare Spending
• Specialty accountable care organizations (ACOs)
A common element in all the value-based reimbursement models for oncology was a drug spending reduction goal. The models aimed to decrease prescription drug spending and utilization because medication costs represented the greatest cancer episode cost.
Drug spending, including chemotherapy, accounted for 78 percent of the costs for a 6-month breast cancer episode, researchers found after analyzing commercial claims data for over 1,300 cancer episodes.
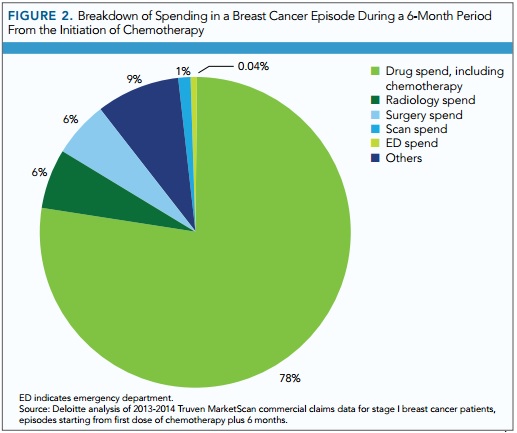
Source: Evidence-Based Oncology
Most of the breast cancer episode costs variation also stemmed from drug spending, followed by surgery and radiology.
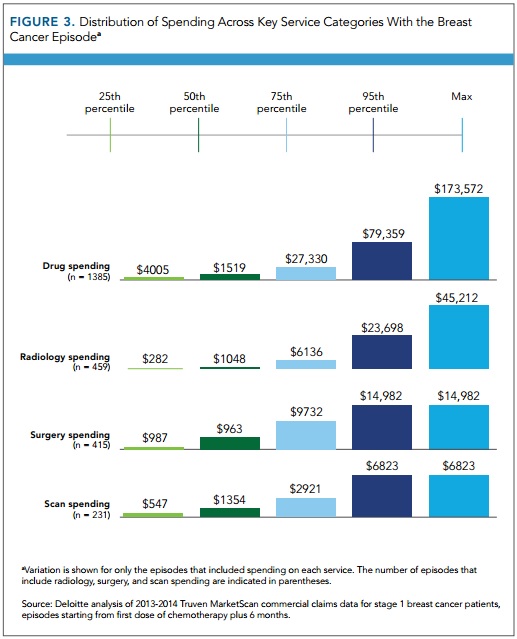
Source: Evidence-Based Oncology
READ MORE: How Alternative Payment Models Decrease Cancer Care Costs
With drug spending representing the greatest opportunity for cancer care cost reductions, the four value-based reimbursement models aimed to lower treatment costs by implementing either clinical pathways or bundled payments.
All stakeholders interviewed reported implementing a value-base reimbursement model that used clinical pathways to guide providers to the most cost-effective cancer treatments.
Providers engaging with the model had to adhere to the pathway between 70 and 85 percent of the time to qualify for financial incentives. The adherence range also gave providers flexibility for necessary care variations based on patient characteristics, preferences, and new treatments.
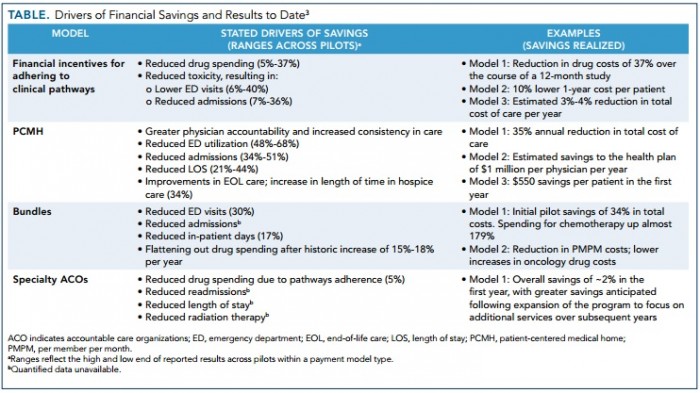
The clinical pathway model generated significant healthcare cost declines, especially for drug spending and healthcare utilization. Drug costs decreased between 5 and 37 percent.
Reduced toxicity also resulted in 6 to 40 percent less emergency department visits and 7 to 36 percent fewer hospital admissions.
Source: Evidence-Based Oncology
READ MORE: Preparing the Healthcare Revenue Cycle for Value-Based Care
Stakeholders reported that the clinical pathway models substantially influenced prescribing patterns. Providers were less likely to use off-pathway drugs because prescribing them would require additional prior authorizations.
However, some interviewees expressed concerns about the value-based reimbursement method. Some providers resisted clinical pathway adoption because they did not want to face a situation where they could not use an innovative treatment that was not yet approved for a clinical pathway.
Bundled payments also emerged as a common method for reducing cancer care costs. Most interviewees participating in bundled payment models stated that drug costs were part of the bundle which covered services anywhere between one month to two years.
The oncology bundled payment models resulted in the following cost and utilization reductions:
• 30 percent less emergency room visits
• 17 percent decrease in inpatient days
• Drug spending stabilization after a historic increase between 15 and 18 percent per year
However, almost all of the stakeholders mentioned that they were not participating in a two-sided financial risk model.
Despite healthcare savings, some interviewees voiced concerns about how financial incentives might discourage novel treatment use, especially since cancer drugs tended to be expensive. Other stakeholders also argued that the bundled payment model did not account for typical cancer care variations, especially for cases with low patient volumes.
To dispel stakeholder concerns and promote financial risk adoption, health plan interviewees said they were experimenting with new bundled payment model designs that boost provider flexibility with using new, expensive treatments. The designs included basing bundles on cancer stage and biomarker status, regularly adjusting bundle prices, and adding stop-loss provisions to decrease financial risk after spending exceeds a threshold.
Providers interviewed also stated that they are considering moving to a two-sided financial risk oncology model to earn maximum value-based incentive payments under MACRA.
The two-sided risk Oncology Care Model qualifies for an automatic 5 percent Medicare payment boost on top of potential shared savings payments. Providers wished to leverage the additional reimbursement by moving to the two-sided financial risk track of the model.
Using the clinical pathway and bundled payment methods, the patient-centered medical home and specialty ACO models also produced healthcare cost savings. The cost reductions primarily stemmed from decreased drug spending and healthcare utilization.
The value-based reimbursement models generated the following results:
• Patient-centered medical home reduced emergency department utilization between 48 and 68 percent
• Patient-centered medical home decreased admissions between 34 and 51 percent and length of stay between 21 and 44 percent
• End-of-life care improved under the patient-centered medical home because length of time in hospice increased by 34 percent
• Specialty ACOs dropped drug spending through pathway adherence by 5 percent
• Admissions, length of stay, radiation therapy rates fell for specialty ACOs but quantified data was unavailable
Based on the study’s findings, researchers suggested that stakeholders build on the oncology-focused value-based reimbursement models and add quality measures that reflect the value of innovation. Quality measures should also incorporate more patient needs to account for novel treatment value.
Researchers also recommended that clinical decision support tools use multiple patient variables and healthcare cost comparisons to help guide providers to the most valuable cancer care options.
