CMS Extends Deadline for Bundled Payment Models Participation
Providers who began operating in Models 2, 3, and 4 starting in October 2013 will be able to extend their participation in these bundled payment models until September 30, 2018 even though it was originally scheduled to end in September of 2016.

The federal government especially the Centers for Medicare & Medicaid Services (CMS) have long focused on reducing healthcare spending and implementing alternative payment models such as pay-for-performance initiatives. Bundled payment models, for instance, have become more prominent through CMS and the healthcare industry in recent years.
CMS established the Bundled Payments for Care Improvement initiative and has recently announced that participants of this program will be allowed to apply for taking part in Models 2, 3 and 4 through September 30, 2018.
Dr. Patrick Conway, Acting Principal Deputy Administrator and Chief Medical Officer, wrote for the CMS Blog that the awardees or providers who began operating in Models 2, 3, and 4 starting in October 2013 will be able to extend their participation in these bundled payment models until September 30, 2018 even though it was originally scheduled to end in September of 2016.
Conway explained that by extending the program of bundled payment models, CMS will be able to more rigorously evaluate the success of the Bundled Payments for Care Improvement initiative and whether it has brought a decrease in healthcare spending while improving quality care.
Starting earlier this month, the bundled payment models program had a total of 1,522 participants with 321 Awardees and 1,201 Episode Initiators, Conway mentioned. Models 2, 3, and 4 have a total of 48 clinical episodes providers can decide upon when attempting to design new and innovative healthcare delivery programs, reduce medical care costs, and improve the quality of patient care.
Conway goes on to say that bundled payment models enable providers to receive reimbursement for a continuum of healthcare services during an episode of care such as payment for hip replacement surgery or treating heart disease by installing a pacemaker or other medical device. This leads multiple providers to work together and improve care coordination during hospital stays and after discharge.
Both federal agencies like CMS and the healthcare industry are concerned over the reduction of healthcare costs, which is why bundled payment models are being implemented. Bundled payments are expected to help strengthen care coordination in an effort to save medical costs.
In the Bundled Payments for Care Improvement initiative, CMS and providers are specifically serving Medicare beneficiaries. When it comes to Medicare beneficiaries, about 67 percent of these patients have multiple medical conditions, which takes up a total of 94 percent of Medicare costs.
Additionally, Medicare beneficiaries who are minorities end up with higher rates of disease, lower quality care, and a general restriction to healthcare access, according to The CMS Blog.
It is vital to understand disparities of this kind so that new healthcare delivery and reimbursement systems such as bundled payment models can be created to address these issues.
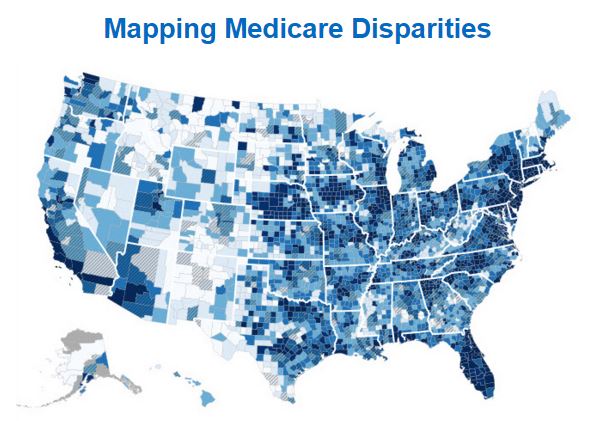
In order to truly reform our healthcare system, it is vital for CMS and other state or federal agencies to work to identify health disparities and close gaps in care. Last month, the CMS Office of Minority Health (OMH) released the Mapping Medicare Disparities (MMD) Tool.
“Understanding disparities and their geographic variations is important to inform policy decisions and to identify populations and localities to target for interventions,” states The CMS Blog. “As health care delivery system reform continues, the Centers for Medicare and Medicaid Services (CMS) has an important opportunity and a critical role to play in promoting health equity.”
“In September 2015, the CMS Office of Minority Health (OMH) released the first CMS Equity Plan for Improving Quality in Medicare. In March 2016, CMS OMH launched a newly developed interactive tool to increase understanding of geographic disparities in chronic disease among Medicare beneficiaries.”
“The Mapping Medicare Disparities (MMD) Tool presents health-related measures from Medicare claims by sex, age, dual eligibility for Medicare and Medicaid, race and ethnicity, and state and county. It provides users with a quick and easy way to identify areas with large numbers of vulnerable populations to target interventions that address racial and ethnic disparities.”
“The MMD Tool is expected to help government agencies, policymakers, researchers, community-based organizations, health providers, quality improvement organizations, and the general public analyze chronic disease disparities, identifying how a region or population may differ from the state or national average.”
In order to truly make a difference for Medicare beneficiaries, CMS will need to consider minority populations when it comes to developing new healthcare payment initiatives like bundled payment models or the Medicare Shared Savings Program.