CMS’s Quality Measurement Development Plan Supports MIPS, APM
“CMS is committed to reducing provider burden through the use of measures aligned across federal and private-payer quality reporting programs."

- 2016 may be an especially good year for healthcare providers when it comes to matters of revenue cycle management.

The Centers for Medicare & Medicaid Services (CMS) recently posted a 63-page Measure Development Plan, a strategic framework for future clinician quality measurement development that aims to alleviate provider burden.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) supports healthcare’s transition from volume to value with the new Merit-based Incentive Payment System (MIPS) and incentives for healthcare providers to participate in alternative payment models (APMs).
“The Measure Development Plan outlines how we’ll draw from our quality measure development experience to build a measure portfolio for MIPS and APMs. Existing measurement strategies, policies, and principles will guide our efforts," explains Kate Goodrich, MD, MHS, CMS’s Director at the Center for Clinical Standards & Quality, on CMS’s official blog.
“The Measure Development Plan describes how CMS will work collaboratively with federal and state partners and private payers to create an aligned set of measures that reduces provider burden. The plan also describes resources and activities that can contribute to the development of measures applicable to a wide variety of stakeholders.”
“These programs move the Medicare program and our overall health care system toward paying for the quality rather than the quantity of care delivered to patients.”
The Measure Development Plan concentrates on numerous identified gaps in currently implemented quality measure sets for PQRS, VM, and the EHR Incentive Program, Goodrich says.
CMS offers a series of recommendations for how these presented problems can best be addressed.
“Future measure development will prioritize person-[centered] and caregiver-centered experience of care, patient-reported outcomes and patient health outcomes, communication and care coordination, and appropriate use of resources across six quality domains.”
CMS identifies these quality domains as follows:
- Clinical Care
- Safety
- Care Coordination
- Patient and Caregiver Experience
- Population Health and Prevention
- Efficiency and Cost Reduction
Goodrich says any comments, questions, or thoughts regarding the aforementioned information are due either online, via email, or via snail mail by March 1.
Selected highlights from CMS’s Quality Measurement Development Plan
"Building on the principles and foundation of the Affordable Care Act, the Administration announced a clear timeline for targeting 30 percent of Medicare payments tied to quality or value through alternative payment models by the end of 2016 and 50 percent by the end of 2018,” says CMS.
“These are measurable goals to move the Medicare program and our healthcare system at large toward paying providers based on quality, rather than quantity, of care.”
“The passage of the Medicare Access and Children’s Health Insurance Program (CHIP) Reauthorization Act of 2015 (MACRA) supports the ongoing transformation of healthcare delivery by furthering the development of new Medicare payment and delivery models for physicians and other clinicians.”
One of CMS’s quality initiatives includes measure development. First released two years ago and updated earlier this year, the CMS Quality Strategy outlines 6 goals to help improve quality of care, including making care more affordable.
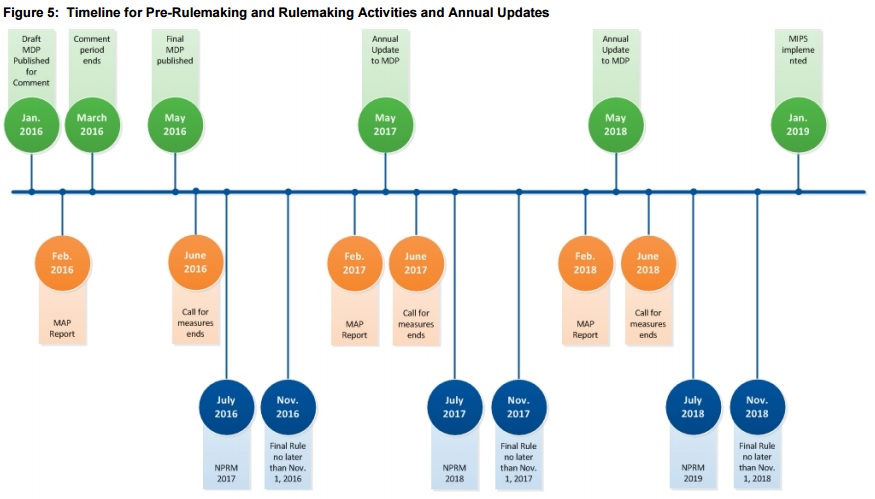
CMS additionally presents a “Measure Development Timeline,” outlining key dates from 2016 to the beginning of 2019.
Updates will be either be published annually or “otherwise as appropriate,” CMS says, to report on items such as newly identified measure gaps and new challenges.
“CMS is committed to reducing provider burden through the use of measures aligned across federal and private-payer quality reporting programs. We stress harmonization of data elements and specifications among measure developers, whose cooperation and sharing are essential to creating aligned measures,” CMS writes.
“Toward that end, we also intend to leverage the optional pre-rulemaking process and MAP review for MIPS and to participate with other stakeholders in efforts that promote measure alignment. This draft MDP acknowledges the associated challenges and identifies opportunities for measure developers to share information to reduce duplication of efforts.”
“The successful implementation of the MDP depends on collaboration with multiple stakeholders to develop measures that are meaningful to patients and providers and can be used across payers and healthcare settings.”
