Healthcare C-Suite, Earned Incentive Compensation Down in 2016
Most healthcare executives saw their pay decrease in 2016, especially after earned incentive compensation dropped, an AMGA survey found.

Source: Thinkstock
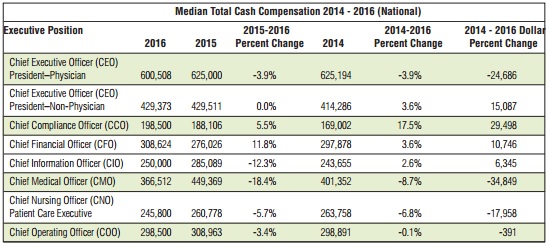
- Median healthcare CEO compensation in terms of total cash value remained relatively the same for non-physician executives in 2016, while physician CEOs faced a 3.9 percent reduction, a recent AMGA Consulting survey found.
The survey of 78 medical groups also showed that most C-suite positions experienced compensation reductions in 2016, stemming from less executives earning value-based financial incentives.
“The 2016 survey indicates that leadership compensation is not simply increasing by a consistent 3 percent or 4 percent year-over-year,” stated Tom Dobosenski, AMGA Consulting President. “The survey results show that factors such as the magnitude of incentive compensation, executives’ achievement of those metrics, and the available labor force for some specialized positions are important.”
Healthcare Chief Medical Officers saw the greatest median cash compensation decrease in the past year with an 18.4 percent reduction, followed by Chief Information Officers with a 12.3 percent decline in cash compensation, Chief Nursing Officers with a 5.7 percent decrease, and Chief Operating Officers with a 3.4 percent reduction.
Chief Medical Officer and Chief Information Officer compensation particularly took a dive in 2016. The healthcare executive positions had experienced significant pay increases in years past. According to last year’s survey, both positions faced compensation increases between 11 percent and 17 percent from 2014 to 2015.
Source: AMGA
READ MORE: Driven by Specialists, Physician Compensation Rates Rise 3.1%
AMGA researchers attributed some year-over-year compensation differences to survey participation changes, but the industry group added that value-based incentive compensation also played a major role in pay decreases.
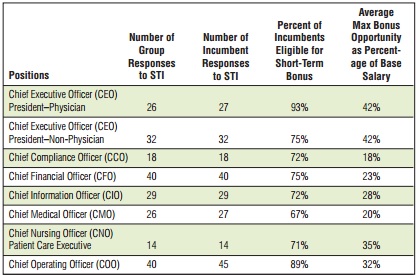
Last year’s survey revealed that about 62 percent of healthcare C-suite executives received some incentive compensation in 2015.
However, the number of executives earning incentive compensation in 2016 dropped to just 48 percent, even though about two-thirds of incumbent executives were eligible for some type of short-term incentive compensation or financial bonus.
In 2016, medical groups reported that their healthcare C-suite executives were eligible for an average maximum financial bonus of 18 percent to 35 percent of their base salary. Although, healthcare CEOs had the opportunity to earn financial bonuses of 42 percent of their base salary.
Source: AMGA
Based on how much healthcare executives could have earned in financial bonuses, AMGA noted that the decrease in the number of C-suiters realizing financial bonuses likely affected total cash compensation.
READ MORE: How Value-Based Reimbursement Affects Physician Productivity
“It may be the case that, similar to physician compensation, executive incentives are evolving more and more to align with strict outcomes measures, and those measures include a greater ‘stretch’ component for maximum payout,” Wayne Hartley, AMGA Consulting Vice President, and Aaron Dobosenki, AMGA Consulting Direction, wrote in an accompanying article.
While many healthcare executives saw their compensation decline, the survey showed that some C-suite positions enjoyed pay increases in 2016.
Chief Financial Officers experienced the highest median total cash compensation boost with 11.8 percent. However, compensation increases may have stemmed from position changes, AMGA pointed out. The executive position used to be divided between a Vice President of Financial Positions and the Chief Financial Officer, but many medical groups eliminated the VP-level position.
Chief Compliance Officers also saw a compensation increase in 2016. The executive position experienced a 5.5 percent boost in median total cash compensation between 2015 and 2016, contributing to a 17.5 percent increase from 2014 to 2016.
“We suspect this growth is linked to the clear focus on regulatory issues across the industry and the demand for a limited number of medical group compliance professionals,” wrote Hartley and Dobosenki.
READ MORE: Preparing the Healthcare Revenue Cycle for Value-Based Care
Similarly, more specialized positions were added to the 2016 survey that had high valuations due to their unique skill sets required and a limited employment pool. In the past year, more medical groups hired Directors of Physician Compensation and Directors of Care Coordination/Care Management.
Physician compensation directors received a median total cash compensation of $144,700 in 2016. AMGA pointed out that the position’s valuation was greater than the national median compensation for Director of Finance/Controller, which was at $143,500 last year.
“Such a valuation may indicate the importance of a central leader for physician compensation at a time when physician compensation is increasingly linked to quality and other value-based metrics (and appreciates the associated increase in administrative and record-keeping requirements to ensure appropriate credit to physicians),” the article stated.
As value-based reimbursement adoption gains momentum, more medical groups are also employing care coordination and case management directors. The position made its debut on the annual AMGA survey with a median total cash compensation of $115,750 in 2016.
“While a longstanding position in hospital settings, the director of care coordination/case management has become more prevalent in medical groups with the expansion of population health initiatives,” stated Hartlet and Dobsenski.
“We anticipate this position will continue to grow in popularity as more emphasis is placed on patient experience and clinical outcomes in the outpatient setting.”
Between compensation reductions and new positions, the survey indicated that healthcare executive compensation determinations are not as simple in a value-based reimbursement landscape.
Value-based payment structures are prompting some medical groups to incorporate incentive compensation into their executive pay structures. But successfully managing the transition to more value-based incentive compensation has proven to be a difficult task for some executives.
Additionally, many medical groups are seeking and implementing value-based care capabilities, such as increased care coordination and population health management adoption. To manage these new initiatives, the organizations are placing specialized individuals in charge to ensure success.
“As medical groups and integrated systems of care transition to value, it is imperative that boards and compensation committees have the necessary data to make well-informed decisions on compensation for their leaders,” said Donald W. Fisher, PhD, CAE, AMGA President and CEO. “The survey data are an important resource for leaders as they make the difficult decisions that balance financial stewardship with fair and competitive market-based pay.”
