ICD-10 Claim Denial Rate Remains Low among Most Providers
The ICD-10 claim denial rate is low and seems to be at a minimum among most hospitals and healthcare providers.

- It seems that the ICD-10 implementation has not had a very negative effect on the ICD-10 claim denial rate, which hasn’t risen much since the October 1 deadline. For example, RelayHealth Financial, a revenue cycle management solutions provider, announced in a press release data on their ICD-10 claim denial rate between October 1, 2015 and February 15, 2016.

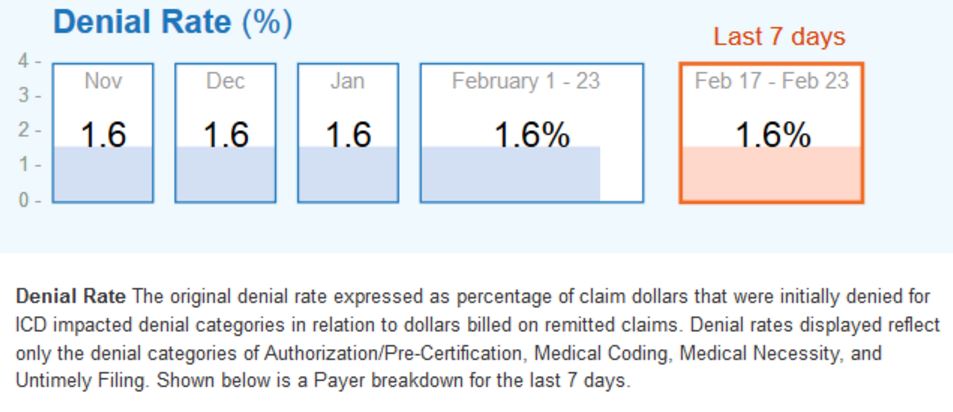
The report includes information on more than 262 million claims that were processed during the four and a half month period. The organization found that only 1.6 percent of ICD-10 claims were denied out of all processed through the revenue cycle management tools. A total of 630,000 healthcare providers and 2,400 hospitals have used RelayHealth Financial tools and positioned $810 billion in claims through these revenue cycle management solutions.
The 1.6 percent ICD-10 claim denial rate has not differed significantly since November, the company reports. About $12.9 billion in medical claims has been denied since the ICD-10 implementation deadline of October 1, 2015.
“The good news is that we’re not seeing a marked increase in claim denial rates, and there is heightened interest in denial management and prevention,” Marcy Tatsch, Vice President and General Manager of Reimbursement Solutions for RelayHealth Financial, said in a public statement.
“The bad news is that as many as 1 in 5 claims is still denied or delayed–which can mean a dip of as much as 3 percent in a hospital or health system’s revenue stream. While it’s important to keep monitoring those KPIs that are monitored on RelayHealth Financial’s Denials Dashboard, healthcare providers should now ramp up their broader denial prevention and management efforts.”
RelayHealth is now offering an online website to help healthcare providers better understand, prevent claim denials, and reduce their ICD-10 claim denial rate. To visit the website, click here. This online resource has white papers, case studies, and a webinar outlining some essential advice for best practices at preventing ICD-10 claim denials.
Nonetheless, the ICD-10 claim denial rate is low and seems to be at a minimum among most hospitals and healthcare providers. Last week, the Centers for Medicare & Medicaid Services (CMS) even declared that their ICD-10 claim denial rate was only 0.07 percent in the fourth quarter of 2015. There were also 0.07 percent of ICD-9 claims rejected at the end of 2015.
One survey from Porter Research and Navicure showed that, after the October 1 ICD-10 implementation deadline, 60 percent of survey takers didn’t seen any impact on their monthly revenue while for one-third of those polled, monthly revenue did decline by up to 20 percent. For 2015’s fourth quarter, CMS did deny 9.9 percent of total claims submitted.
Many hospitals and medical providers were concerned after the October 1 deadline that they may suffer from revenue loss due to claim denials by CMS and other health payers. However, the results seem to show that most were prepared for the new diagnostic coding set.
CMS also stepped forward in helping solve the many issues that cropped up after the ICD-10 implementation deadline took effect. This led to fewer claim denials and problems related to claims processing than once projected.
CMS Acting Administrator Andy Slavitt explained that the transition to the ICD-10 diagnostic coding set was similar to Y2K, as it could create serious problems for the healthcare industry if not implemented correctly. The ICD-10 coding set could have led to disastrous results for the revenue of hospitals and clinics if these organizations were not adequately prepared.
“For people in the health care industry, it was being compared to Y2K, a transition with the potential to create chaos in the health care system,” Slavitt wrote in the CMS blog.
“One representative from the physician community told me that he was concerned that half of physicians in the country wouldn’t be ready by the October 1 date. The thought of physicians in small, rural practices unable to run their practices had my complete attention. It also brought home that we are responsible for more and increasingly complex implementations – from HealthCare.gov to ICD-10 to new physician payment systems.”
While many feared that rural clinics and smaller medical practices wouldn’t fare well under the ICD-10 implementation, CMS has been responsible for helping providers get through some complex transitions such as the Affordable Care Act’s health insurance exchanges.
There are four specific elements that CMS utilized when it comes to transitioning to the new ICD-10 coding set. These include a greater focus on the consumer, collaborating more among stakeholders and the healthcare community, responding quickly and effectively to ICD-10 challenges or issues, and using metrics to keep claim processing and denial rates in check.
“With preparation, planning, a focus on the customer, collaboration, clear accountability, and metrics, the dire Y2K fears didn’t come to pass. Instead, ICD-10 became like what actually occurred on Y2K,” Slavitt explained in the article.
Now that the ICD-10 implementation deadline has passed and revenue seems to remain stable among most healthcare providers, the next focus of hospital executives is to remain dedicated to value-based care payments and bundled payment models. Many are looking at workflows and patient care improvements that could lead to greater reimbursement.
The future will show where the healthcare industry will move with regard to improving patient care and health outcomes while working to reduce wasteful spending and increase revenue.
Image Credits: RelayHealth Financial