Payment Reform Strengthens Patient-Centered Medical Home
The patient-centered medical home concept is a model in which physicians work to coordinate high-quality care and ensure greater patient satisfaction.

- The health payer industry and the federal government including the Centers for Medicare & Medicaid Services (CMS) have positioned hospitals, clinics, and medical practices to adopt necessary healthcare payment reform. Alongside accountable care organizations, bundled payments, and value-based care reimbursement, the patient-centered medical home stands as a real boon to healthcare payment reform.

The patient-centered medical home has transformed physician reimbursement and shown to decrease medical costs while improving the quality of patient care. The Primary Care Development Corporation announced in a press release that it has assisted 200 primary care practices toward obtaining the National Committee for Quality Assurance (NCQA) patient-centered medical home (PCMH) recognition.
Quality care incentives through Medicare, Medicaid, and commercial payers are making headway among providers committed to healthcare payment reform. The patient-centered medical home concept is a model in which physicians work to coordinate high-quality care and ensure greater patient satisfaction. These type of models of care are seen as a clear pathway toward receiving financial incentives from public and private payers.
In the state of New York, the Delivery System Reform Incentive Payment program (DSRIP) requires all patient-centered medical home models to obtain the highest level of recognition, according to the release. Currently, the Primary Care Development Corporation is helping a number of medical homes achieve this status.
“PCDC’s mission is to ensure access to quality primary care for every family in every community,” Primary Care Development Corporation CEO Louise Cohen said in a public statement. “The medical home model is widely accepted as how primary care should be organized and delivered – and I am proud that we have now helped 200 practices provide more coordinated, patient-centered care to hundreds of thousands of patients.”
Additionally, the organization is seeking ways to expand access to primary care in various communities around the nation. Two medical practices located in New York City under the Mount Sinai Doctors Faculty Practice name achieved PCMH Level 3 recognition from NCQA after receiving consultation and coaching from the Primary Care Development Corporation.
These two medical practices handle more than 13,000 patients on an annual basis, which includes at least 1,300 Medicaid beneficiaries. At this moment in time, the organization is assisting two other Mount Sinai primary care practices to obtain the patient-centered medical home recognition.
“The medical home model is essential to Mount Sinai’s strategy of transforming how health care is delivered in the communities we serve,” Burton Drayer, MD, CEO, Mount Sinai Doctors Faculty Practice and Dean for Clinical Affairs, Icahn School of Medicine at Mount Sinai, stated in the press release. “PCDC’s leadership and expertise has helped us strengthen our practices, and we are delighted that a Mount Sinai faculty practice is PCDC’s 200th successful NCQA PCMH recognition.”
There are specific protocols that the Mount Sinai practices have taken to achieve the NCQA patient-centered medical home status. One includes notifying primary care physicians when a patient visits an emergency room or is admitted to the hospital.
Additionally, patients were introduced to vital community resources and social services. The two medical practices also made sure to monitor patients when out of the hospital and connect those who frequently visit the emergency department with stronger primary care prevention.
With these systems in place, the primary care practices were actually able to reduce the number of patients visiting emergency rooms and being admitted to the hospital, according to the release. The patient-centered medical home concept was able to help these providers improve the quality of care as well as lower overall medical spending by decreasing the amount of times acute care services are used.
The Primary Care Development Corporation has spent the last five years coaching community health centers, clinics, special needs providers, and private physician practices how to achieve the patient-centered medical home recognition afforded by NCQA.
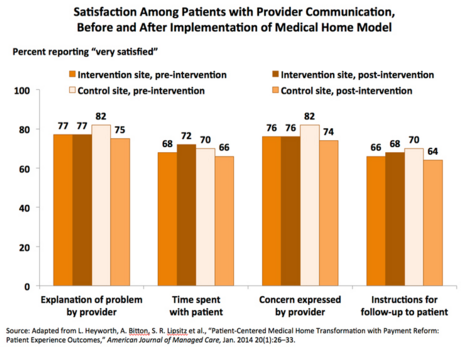
The Commonwealth Fund discovered in a study that patient satisfaction is high in patient-centered medical homes that adopt physician payment reforms. Even communication between doctors and patients was enhanced.
These finding run in the opposite direction of other studies that have shown that patient satisfaction is negatively impacted in the short term due to the adoption of the patient-centered medical home model.
“This investigation did not find evidence that implementation of the patient-centered medical home, when combined with lean changes and provider payment reform, negatively affected patients’ experiences,” the report stated.
“In fact, the findings suggest that this delivery model may bolster patient–provider relationships. Physicians at the intervention site may have felt reduced time pressure as a result of the workforce changes and their new payment structure, perhaps freeing up time for more in-depth and better-quality conversations with patients. Practices interested in the PCMH model, the authors say, may want to consider reforming physician payment early in the transformation process.”
Patient satisfaction ratings increased by 6 percent, the study found. In particular, physician communication was seen more favorably when using the patient-centered medical home concept. The study uncovered that physician payment reform is key for developing the patient-centered medical home and for revolutionizing patient satisfaction.
As healthcare payment reform continues to be implemented across the country, programs like accountable care organizations and patient-centered medical homes will be a primary means toward achieving value-based care status.