Physicians List Top 5 Value-Based Payment Success Factors
"Physicians are genuinely concerned about the time needed to transition to value-based payment and want to ensure that their efforts translate to care improvement."

- Physicians say lack of time is one of the leading obstacles they face regarding value-based care delivery, according to a study from the American Academy of Family Physicians (AAFP).

One-third of family physicians are actively pursuing value-based payment opportunities, confirmed the Humana-sponsored survey of 5,000 active AAFP members.
Another 19 percent are reportedly waiting it out until they have a clearer sense of what the broader value-based payment picture looks like. In the meantime, this 19 percent is indeed working to further develop their value-based competencies, stated AAFP.
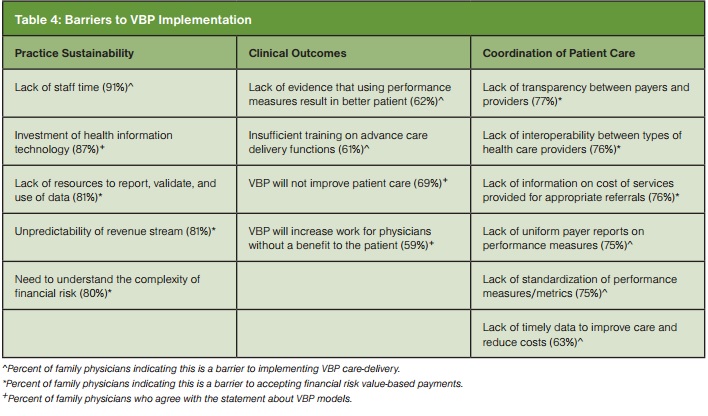
Physicians reportedly are quite dubious about how value-based payments will affect care outcomes, confirmed AAFP. Time is a reported major hindrance when it comes to value-based care implementation efforts.
Sixty-nine percent of physicians said value-based payments will not advance patient care. Additionally, 59 percent believe value-based payments will increase their workloads without any clear patient advantage.
According to Humana’s press release, the AAFP’s research was completed “considering the urgency” of the Department of Health and Human Services’ “fast approaching” goal to tie 50 percent of fee-for-service Medicare payments to value-based payment models by 2018.
Additionally, the goal for next year – right around the bend, nonetheless – is to tie 30 percent of Medicare payments to quality and value via alternative payment models, such as accountable care organizations.
The healthcare industry aims for progress as 2016 nears
This goal is clearly a massive undertaking. Naturally, many big names in healthcare have been speaking out regarding how to reach such goals as the clock ticks onwards.
“We are pleased with the progress towards transforming our healthcare system into one that is better, smarter, and results in healthier people. But, there is more work to be done. The last five years have seen the most positive delivery system improvements in our nation’s history, and we are committed to accelerating that progress,” recently stated Patrick Conway, MD, MSc, Chief Medical Officer at the Centers for Medicare & Medicaid Services (CMS).
“We are dedicated to using incentives for higher-value care, fostering greater integration and coordination of care and attention to population health, and providing access to information that can enable clinicians and patients to make better-informed choices,” said Sylvia M. Burwell, HHS Secretary, last January regarding the timeline’s overview.
“We’re all partners in this effort focused on a shared goal,” said Douglas E. Henley, MD, AAFP’s Executive Vice president and Chief Executive Office, earlier this year. “Ultimately, this is about improving the health of each person by making the best use of our resources for patient good. We’re on board, and we’re committed to changing how we pay for and deliver care to achieve better health.”
Key findings from AAFP’s research study
- Family physicians have contracts with a substantial number of health plans. Sixty-one percent of family physicians receive payment from seven or more health plans, and of that 38 percent receive payment from 10 or more.
- A substantial proportion of family physicians remain uninformed regarding value-based payments. One in four don’t know or are not sure of their practice’s status or current strategy toward value-based payments, and 32 percent don’t know if value-based payment models are available in their market. Among those participating in value-based payments, 33 percent didn’t know how the payments were being distributed within their practices (e.g., administration, physicians).
- The necessary time commitment is a major concern among physicians. More than 90 percent of physicians surveyed indicated lack of staff time as a barrier to implementing value-based care delivery.
- Health information technology investment and necessary resources to report, validate and support data affects practice sustainability. Eighty-seven percent of practices said they will have to make substantial investments in health information technology to be successful in a value-based payment model. In addition, 81 percent provided that lack of resources to support reporting, validation and use data also impacts their practice’s sustainability.
Physicians list their top 5 value-based payment model success factors
- Practice sustainability – 92 percent
- Clinical outcomes – 91 percent
- Physician and staff morale – 87 percent
- Coordination of patient care – 86 percent
- Cost savings for physician’s practice – 84 percent
 “The results of this study tell us that physicians are genuinely concerned about the time needed to transition to value-based payment and want to ensure that their efforts translate to care improvement,” said Roy A. Beveridge, MD, Humana’s Chief Medical Officer, in relation to the aforementioned findings.
“The results of this study tell us that physicians are genuinely concerned about the time needed to transition to value-based payment and want to ensure that their efforts translate to care improvement,” said Roy A. Beveridge, MD, Humana’s Chief Medical Officer, in relation to the aforementioned findings.
“The health care industry would benefit from improving its understanding of physician needs and how they can best alleviate burdens. Partnering with the AAFP through this study gives us an understanding of the unique needs of the family physician to accelerate their journey to value and realize improved care outcomes.”
“It is encouraging to see that many physicians are moving toward value-based payment, but what’s clear from this study is that there is significant work to be done,” stated Wanda Filer, MD, MBA, AAFP President.
“Accelerating the adoption of value-based payment will require a commitment from physicians and health plans to share in the responsibility of delivering value-based payment.”
