Physicians Report 4 Factors of Value-Based Payment Success
92 percent of surveyed family physicians say practice sustainability is the leading factor in determining value-based payment success.

- Are value-based payment models garnering favorable reviews or mere disdain from physicians? A new Value-Based Payment (VBP) Humana-funded study aims to answer this perhaps simultaneously simple yet heavy-handed question.

Survey data was collected last June from over 600 members of the American Academy of Family Physicians (AAFP). The report assessed general perceptions of VBP models.
Key findings about PCMHs, ACOs
- Of those practices surveyed, over 70 percent include either a nurse practitioner or a physician assistant. Over a quarter include a care manager.
- Forty percent confirmed their practices are a designated patient centered medical home (PCMH); another 12 percent confirmed they submitted applications.
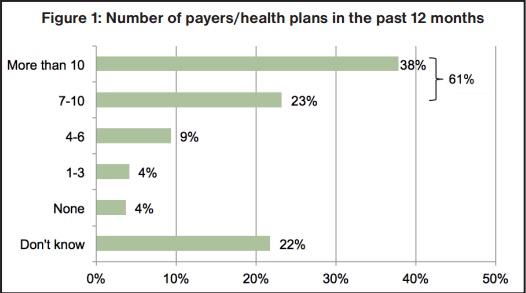
- Thirty-eight percent are reportedly tied to Accountable Care Organizations (ACOs). Additionally, over 60 percent said they had submitted claims to at least 7 payers over the past year.
Key findings about overall VBP approaches
- According to collected data, a third of practices asserted they are “actively pursuing” VBP.
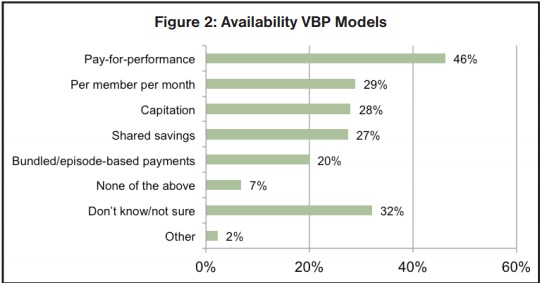
- Pay-for-performance programs are reportedly available within a given market only about half of the time.
- One-third were utilizing remaining payment models, albeit not as often.
- Over a quarter of those surveyed said they are indeed knowledgeable that payments are being received by practice administration but remain undistributed to physicians. Another quarter confirmed awareness of their practice distributing payments to physicians.
- Regardless, 1 in 3 were simply "not aware” of how payments were being managed by their practice, something that researchers said “should be noted.”
Physicians point to 4 key elements of VBP success
The vast majority of physicians – up to 92 percent – asserted VBP model success can be verified by 4 leading factors: practice sustainability, clinical outcomes, physician and staff morale, and patient care coordination.
Family physicians additionally noted a slew of obstacles that hinder their over VBP success. Leading barriers include lack of staff time, the investment of health information technology, insufficient resources for data reporting and validation, and a general lack of predictability when it comes to revenue stream.
80 percent confirmed they simply lack understanding when it comes to the overall complexity levels associated with financial risk. Sixty-nine percent said VBP “will not improve patient care.” Over half confirmed physician workloads will increase because of VBP without any tangible benefit to patients.
Regarding patient care coordination, over three-quarters of family physicians claimed there is not only a lack of transparency between healthcare payers and healthcare providers but a lack of interoperability between providers.
Three-quarters also said payer reports lack consistency regarding performance measures. Additionally, over 60 percent of family physicians confirmed there is no timely data available to help slash healthcare costs.

How to best manage in a VBP environment
In light of the aforementioned opinions and perspectives, value-based payments have been a rather hard to ignore key discussion topic within the healthcare industry, especially within the past year or so.
Regarding more positive findings, over half of healthcare executives surveyed earlier by Humana and the Healthcare Financial Management Association (HFMA) confirmed value-based payment programs helped them hit positive return on investment goals.
Over half of senior financial executives said they are working on acquiring the required capabilities to achieve risk-based value success within the next three years. Key focuses include interoperability, business intelligence, real-time data access, and chronic care management.
In other news, The Centers for Medicare & Medicaid Services (CMS) is in the process of applying a value-based payment program under the physician fee schedule tied to budget neutrality.
“[The] effective adoption and use of health information exchange and health IT tools will be essential as these settings seek to improve quality and lower costs through initiatives such as value-based purchasing,” said CMS.
“Medicare, Medicaid, and commercial health plans are all pushing toward paying hospitals and physicians for value, effectively pushing financial risk upon the providers,” stated Joe Kuehn, Advisory Partner at KPMG’s Healthcare & Life Sciences Practice.
“Finance departments will need to prepare to manage these challenges and have better systems to measure performance against established targets including the cost and quality of care for example, so they can manage in this new environment.”
