Price Transparency Still Missing from Hospital Revenue Cycle
Promoting a culture of consumer price transparency starts with the boards of trustees and CEOs and trickles down through all connected hospital revenue cycle management avenues.

- The Affordable Care Act’s (ACA) numerous price transparency provisions are inefficient, says a policy brief from the Pioneer Institute. Hospital executives must make consumer-friendly pricing information a top revenue cycle focus or else the medical billing process will merely fall apart before it even begins.

Under the ACA, hospitals must establish what their standard charges are for items and services and make this information publicly available, said the policy brief’s authors, Barbara Anthony, Senior Fellow in Healthcare, and Scott Haller, Research Associate.
Additionally, guidelines from the Centers for Medicare & Medicaid Services (CMS) mandate hospitals must make the information available if an inquiry arises so consumers can compare prices with ease.
Fifty-four surveyed acute care hospitals nationwide said they are ill-prepared to provide price information to healthcare consumers. The authors pushed for greater regulatory reform to enact change.
Ninety percent of states reportedly fail to provide adequate consumer pricing information, according to the Catalyst for Payment Reform (CPR).
Fifty-six percent of Americans have searched for price information before receiving care, said David Schleifer, PhD, Public Agenda’s Senior Research Associate.
The Pioneer Institute said there is a lack of standardization across hospitals. Healthcare transparency rules apparently vary sizably according to state.
Most healthcare consumers are unaware variation exists, Schleifer said. Healthcare providers, physicians, nurses, and medical billing staff members need to be on board to enact collective change, he asserted.
According to the Pioneer Institute, a sample of how mandates vary across states is as follows:
- California: all hospitals must make their master charge list available to the public and make common costs available upon request
- Florida: cost estimates are provided to patient per request, as per state law
- North Carolina: under state law, a report must be created that compares prices for common procedures at top hospitals and free-standing clinics
- Texas: hospitals must provide estimates at or before patient admittance
- New York: hospitals must either have charges up on their website “or provide a way for consumers to find them”
All surveyed hospitals were covered by the ACA’s requirements regarding price transparency for consumers, the authors said. The only state that did not offer healthcare consumers the right to see price information was Iowa.
Whether or not state laws are in place “does not seem to influence how easy or difficult it is for consumers to obtain price estimates,” they said.
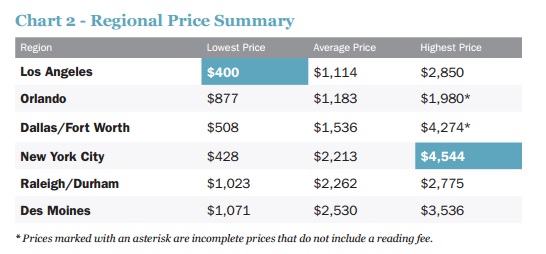
Further complicating matters is that price summary information apparently varied sizably according to region.
According to the Pioneer Institute, “non-disclosure of healthcare prices interferes with the normal operation of market forces and prevents consumers from spending their healthcare dollars wisely."
And because of the growth of high-deductible plans among non-subsidized middle-income healthcare consumers, healthcare price transparency is an even more important issue than ever before, the authors stated.
As the Commonwealth Fund reported early last year, insurance premiums have been increasing at an alarming rate.
“Although the Affordable Care Act offers a platform from which to build, securing a more affordable future will likely require action beyond those reforms, focusing on costs of care, particularly for the privately insured,” the Commonwealth Fund said.
Future initiatives “should focus on prices paid by private insurers, as well as incentives to reorganize the delivery system to improve care experiences and outcomes,” the organization stated.
In 2013, a typical employer-sponsored family insurance premium reportedly ranged from over $13,400 to $20,000 depending on state.
According to the Commonwealth Fund’s 2015 Healthcare Affordability Index, 43 percent of adults with moderate incomes said their deductible was “difficult or impossible to afford.”
The Pioneer Institute reported that under the ACA, deductible amounts may increase by up to $6,500 per person and may top $13,000 per family.
When it comes to transparency, the Pioneer Institute said healthcare consumers are actively trying to figure out how much their care delivery costs and make informed, educated choices.
But when consumers attempt to gather pricing data, it is mostly “impracticable to obtain,” Anthony and Haller asserted.
When researchers called various hospitals nationwide asking for pricing information, they were often met with long wait times.
It took “lots of persistence and diligence on the part of our researchers to obtain price information,” the authors said.
Complete price estimates could not be obtained from 14 of the 54 hospitals. Up to 11 phone calls were made.
Calls were quick to be transferred “back to the operator, billing, financial aid, patient registration, ‘upstairs,’ ‘over there,’ or ‘downstairs,’” they explained.
“Our callers were frequently required to provide medical billing codes about which an ordinary consumer would have no knowledge and further, our staff was often told to call a separate organization altogether to obtain a complete estimate.”
Other physician staff “were quite hesitant to provide price information under the mistaken belief that disclosing price to a prospective patient was not permitted,” they explained.
Price information was generally not available on hospital websites, they revealed. Prices obtained were often nothing more than broad estimates with “wide variations,” they added.
Fifty-seven percent of hospitals took up to 74 minutes to provide the price, or failed to provide a complete price.
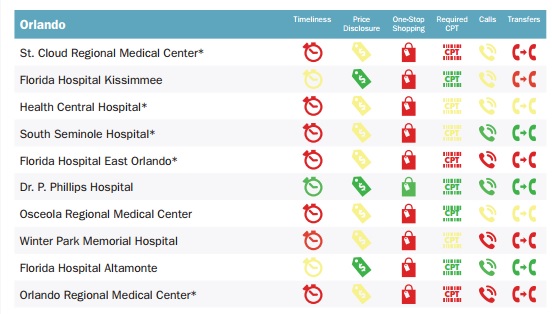
The city of Orlando reportedly received the lowest overall score for timeliness, with 40 percent of its surveyed hospitals taking up to 75 minutes to provide pricing information.
On a positive note, “some hospitals do get it right,” the authors said. Not every hospital sent researchers on a phone transfer whirlwind, expected healthcare consumers to know medical billing codes offhand, or made transfers to wrong departments.
Authors reported the following hospitals received top marks:
- The Iowa Clinic, Des Moines
- Dr. P. Phillips Hospital, Orlando
- Dallas Regional Medical Center
- Cedars Sinai, Los Angeles
- NYU Langone, New York
- Mount Sinai, New York
- Wake Med Cary Hospital, Raleigh/Durham
- Duke University Hospital, Raleigh/Durham
“[Price] transparency can be accomplished, and consumers can access their right to healthcare price estimates,” they concluded. “If some hospitals can do this, it shows that there are systems and protocols in place that can be replicated across the country.”
As far as recommendations to close the gap, the authors advocated going back once more to the ACA drawing board.
“We need to create a national culture of healthcare price transparency. There already exists a legal foundation upon which to build this cultural change,” they said.
“Hospitals working with federal and state governments can lead the way to promote and encourage price transparency as a consumer right. There is a great deal of progress yet to be made and plenty of opportunities for all major stakeholders.”
A review of hospital website content and making sure consumers do not have to spend time digging through medical billing code information to know what their medical bill may look like is key.
“Hospitals should make strong efforts to raise awareness among hospital staff of a consumer’s right to price information and invest in appropriate personnel training to facilitate such requests.”
“Within hospitals, a culture of consumer price transparency should start at the top with boards of trustees and CEOs establishing consumer-friendly and timely access to price transparency information as a priority goal for their institutions.”
Image Credit: [Pioneer Institute] (Chart 2)
Image Credit: [Pioneer Institute] (Orlando)
