Quantify Denial Rates for Smooth Revenue Cycle Management

- A hospital or medical practice’s ability to swiftly and economically process claims and quantify denial rates is critical to ensure smooth revenue cycle management and medical reimbursement. The ability to accurately predict reimbursement income and also address budding claim scrubbing issues will hopefully lead to more timely payments with less time spent processing burdensome paperwork and more time focusing on administering quality value-based care.

A denial rate demonstrates the percentage of claims that payers deny within a certain period of time. This often overlooked percentage offers a tangible numeric insight into the overall effectiveness of revenue cycle management.
Why are claims denied?
Denied claims occur for a variety of reasons. A procedure may have been improperly coded on account of a provider. Care might have been performed outside of a beneficiary’s network. Only twenty-four percent of practices check patient eligibility every visit. An insurer may deem certain care as medically unnecessary or experimental.
Volume of denied claims difficult to pinpoint
There is sizable variation and a general lack of regularity regarding information about the industry average for denied claims. Insurers are often hesitant to release data about how often claims are denied, often stating that such information is private or restricted.
The numbers vary depending on the report. The industry average denial rate may be between five and ten percent, says the American Academy of Family Physicians (AAFP). Meanwhile, a contrasting 2011 Government Accountability Office (GAO) study maintains that up to one quarter of claims are denied.
Some organizations seek to find a definitive number about how frequently claims are denied.
The American Medical Association (AMA) has been publishing report cards since 2008 comparing denial rates from a sampling of over two million electronic claims for almost five million medical services across four hundred and fifty states. Most recently, in 2013, AMA found Medicare denied claims about five percent of time.
AMA also confirmed Aetna’s 2013 denial rate was almost two percent compared with the 2008 denial rate of almost seven percent. United Heathcare’s 2013 denial rate was a little over one percent compared with its 2008 rate of over 2.5 percent. Cigna’s 2013 denial rate was about 0.5 percent compared with its 2008 rate of over three percent.
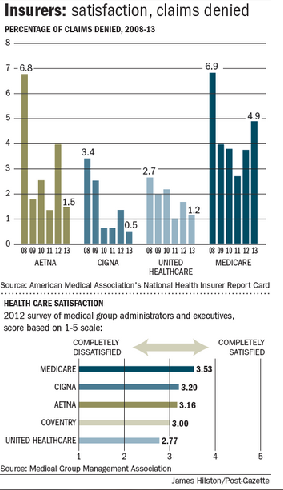
“The wide variation in how often health insurers deny claims, and the reasons used to explain the denials,” says the AMA, “indicates a serious lack of standardization in the health insurance industry.”
Although such reports depict substantial variable and inconsistency from year-to-year, they hopefully can provide a wide-ranging benchmark that requires further definition and focus.
Denial rate calculations
Interpreting denial rates can be compared to golf scores – the lower, the better. Low denial rates imply profitable streams of cash flow.
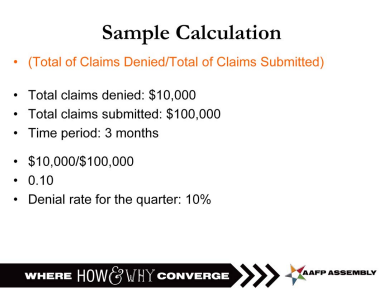
A denial rate can be calculated by taking the total dollar amount of claims that have been denied by payers within a given time period and then dividing by the total dollar amount of claims submitted within the same time period.
Reimbursement rate calculations
Unlike golf scores this time around, the higher the percentage, the stronger the overall performance in the end.
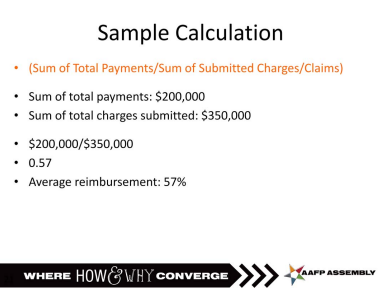
The industry average for the average reimbursement rate a practice collects from total claims submitted is between thirty-five and forty percent.
To calculate the average reimbursement rate, divide the sum of total payments by the sum of the total submitted charges and/or claims.
Payer efficiency and transparency key
According to 2014 data, Medicaid averages forty-four days in accounts receivable. The average for all payers is twenty-six days.
Medicaid’s overall average denial rate was over eighteen percent. The average for all payers was almost seven percent.
The provider collection burden, the percent of allowed amount transferred from the primary to the next responsible party, not including copays and real-time time of service, has increased due to a combination of higher copays, coinsurance, and deductibles.
Last year, data additionally indicated that thirty-eight percent of Medicaid enrollments required mailed paper forms. Paper forms sent via snail mail were not required by national commercial payers.
An appeal a day…
The pen is not mightier than the computer in the realm of claim denial. Avoidable manual errors, simple oversights regarding input, and timing miscalculations cause the rejection of many denials.
Electronic claims are not immune to inaccuracies as automation becomes more mainstreamed. A smeared printed page or an incorrect entry generates similar hindrances as a misread stream of numbers.
As only thirty-five percent of providers appeal denied claims, beginning the appeal process as soon as a denial is received generally leads to greater reimbursement.
Under the Affordable Care Act (ACA), a policyholder can demand an insurer reconsider a denial and follow a subsequent appeal.
The Medical Group Management Association (MGMA) recommends first creating a list of payers’ appeal deadlines since each may have a different timeframe for denial appeals. Possible timeframes may range from forty-five days to three hundred and sixty-five days. Subsequently organizing denials by deadlines will mean urgent appeals are addressed as needed.
Having an appeal letter template in place also expedites the process. Implementation of direct wording from a payers’ written and electronic documentation creates a more effective appeal.
Compatible software tools that allow for streamlining of both denials and appeals can help track a denial’s ongoing progress while seamlessly maintaining reports for denial prevention. Automated processes ensure lower denial rates and fluidity of cash flow.
Determining the patient’s share of cost is the very first step in the life of a claim. Managing information that cannot be concretely quantified is of little benefit for revenue cycle management in the long run.
