4 Key Strategies for Accountable Care Organization Success
Accountable care organizations play a critical role moving the care continuum toward value. But such complex contracting options make it challenging for ACOs to achieve success.

Source: Getty Images
- The passage of the Affordable Care Act sparked many innovative care delivery and payment reform models. One unique model that emerged from this trend was the accountable care organization (ACO).
In this model, groups of doctors, hospitals, and other health care providers voluntarily come together to deliver coordinated, high-quality care to patients. The organizations achieve their goals using a universal budgeting system and value-based reimbursement.
“An accountable care organization is an entity that takes responsibility for the total cost of care for the patients it serves, regardless of whether or not it directly provides that care for their patients,” explained Ed McGookin, MD, chief medical officer of Coastal Medical, an ACO based out of Providence, Rhode Island. “We’re responsible for all the costs of care incurred.”
Like many ACOs, Coastal Medical receives base funding from the Medicare Shared Savings Program. This program and the now-defunct Pioneer ACO model spring boarded the ACO movement, sprouting several offshoots including the ACO Investment Model (AIM) and the Next Generation Accountable Care Organization (NGACO) model, which allowed ACOs to take on significantly more financial risk compared to other iterations of the ACO model.
There is no standard ACO. Each model has a nuanced funding structure and value metrics they report on, and contracts vary from group to group. Some ACOs also include specialists and hospitals while others focus solely on bolstering primary care services.
Increasingly, ACOs have become interchangeable with clinically integrated networks (CINs) as ACOs move away from a legal partnership and towards care coordination.
One of the key measures of success ACOs achieve is improving quality scores, centered around delivering high-quality patient care. ACOs monitor the gaps in care for their members and based on how well the gaps are filled, providers can earn shared savings payments. These payments help fund the comprehensive services offered through the unique care delivery model.
At the core of all ACOs is the mission to deliver high-quality care for lower costs. Despite their differences, many ACOs have common strategies for earning shared savings payments and other value-based incentives, while delivering high-value patient care.
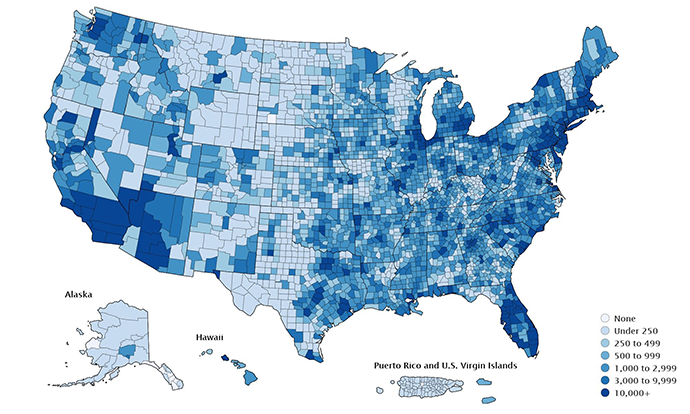
Source: CMS
Expanding Access to Care
For a majority of patients, the traditional notion of care does not work.
Many primary care offices are only open between the hours of 8 a.m. and 4 p.m. and referrals to specialists for challenges that could have been handled by primary care only push patients towards costlier services and even the emergency department.
“Population health compels us to find systems or mechanisms that take care of those who don’t feel that their needs are adequately addressed by that traditional model,” McGookin emphasized.
Practicing what they preach, Coastal Medical looked to their own physician staff first to extend hours.
“We used our clinicians, doctors, and advanced practitioner who wanted to work extra hours and who might like the flexibility of working evenings or weekends if that was helping with some family’s needs,” said McGookin. “We had to create a mechanism to ensure that we have lots of access at Coastal, that patients don’t go elsewhere for services that we can provide.”
The team added after-hours services, weekends and weeknight availability, and alternatives to the emergency department like urgent care.

Stephen Nuckolls, Coastal Carolina Quality Care, Inc.
Source: Coastal Carolina Quality Care, Inc.Similarly, Coastal Carolina Quality Care, Inc. expanded its urgent care. The organization which joined the Medicare Shared Savings Program in 2012 increased staffing and added a new unit for “extended care,” which allowed them to provide many services traditionally reserved for hospitals on site, such as IV fluids and ultrasound.
“We’ve hired emergency room physicians and hospitalists to staff this unit. So, we have the same providers that also work at the hospital. They just work for us part-time,” Stephen Nuckolls, chief executive officer Coastal Carolina Quality Care, Inc. explained. Coastal Carolina Quality Care, Inc. also has an imaging center that can perform ultrasounds typically done in a hospital and staff on call to provide care beyond the traditional hours.
The services may cost the organization a little more to operate, but the savings stemming from an avoidable ambulance ride or a trip to the hospital is worth it. By providing more care on-site, Coastal Carolina Quality Care, Inc. saves patients, resulting in more value-based revenue from its ACO contract.
While some like Coastal Medial are looking inward to reduce costs by leveraging their own physicians, others like Catholic Health Initiatives (CHI) St. Luke’s Health are looking outward to make unique partnerships that accomplish the same goal. The ACO is partnering with vendor organizations to help disseminate information like cancer screening toolkits.
Their national lab partner will donate colorectal cancer screening kits that CHI St. Luke’s can give to their patients. After completing the test at home, patients send the results to the lab partner and the ACO can follow up with any positive results.
“Having that type of partnership beyond the walls of our facility and working with a national lab partner is huge,” articulated Michael Camacho, MPA, division vice president of a clinically integrated network at CHI St. Luke’s Health.
Building Care Teams
Expanding available services requires ACOs to expand their care teams for more coordinated care.
“We focused on coordinating and managing care with nurse care managers so there was somebody helping patients make choices and understand their choices when they were sick or needed services. Over time it evolved to be even more sophisticated,” said McGookin.
Several of these much-needed roles, though, are not necessarily revenue-generating. An administrator or care coordinator often does not produce billable hours or services that the ACO can create a claim for.
But the care coordination work done by these team members can have long-term impacts on patient outcomes. The relationships built through effective care coordination can help ensure patients show up for their appointments, instill confidence in their treatment options, and build trust with their providers. The ACO then becomes the patient’s go-to spot for care rather than the emergency department and other care settings beyond the ACO’s network of providers.

Ed McGookin, MD, CMO, Coastal Medical
Source: Coastal MedicalACOs must make the challenging decision to improve care coordination by growing non-revenue generating positions.
“You have to add more infrastructure costs and personnel. But when there’s a final calculation of performance, then you get your payment,” McGookin asserted.
Luckily, initiatives such as the Medicare Shared Savings Program have the startup funding new ACOs need to enter the market successfully. Funding through these models allows organizations to focus on patient care rather than staying afloat financially. Eventually, shared savings payments also help support new care team members and the coordinated services they provide to patients.
When the work is spread out across a care team, individual providers can focus on their specific elements of care coordination.
“You don’t have to rely on busy, overloaded physicians to do one more thing. They already have too many things on their plate,” Nuckolls emphasized. “We found the most successful way to help them is by adding more members to the team to help close those gaps in care so that everyone’s working at the top of their license.”
Screening tests do not need to be ordered by a physician, he continued. Administrators can handle scheduling, freeing up time for physicians to spend on patient education during the annual wellness visit.
Emphasizing Wellness
Providers in multiple value-based contracts across several payers juggle a variety of quality performance measures to define success. Keeping track of which quality metrics are associated with each patient can be overwhelming and unethical.
Attributing patients to a provider can also be a challenge. Providers are often uncertain who is responsible for filling patients’ gaps in care if the patient is moving between specialists.
One of the simplest solutions to closing gaps in care and understanding who is responsible for closing these gaps is focusing on one standard quality metric: annual wellness visits.
“The focus is really around the primary care physicians and their ability to do wellness visits. That test is the secret sauce,” Camacho insisted. “If you could do wellness visits, you’re helping with attribution, you’re helping with risk scores, you’re helping close quality gaps, all by doing annual wellness visits. There’s a huge emphasis on that.”
“If you could do wellness visits, you’re helping with attribution, you’re helping with risk scores, you’re helping close quality gaps, all by doing annual wellness visits."
Annual wellness visits alone address the bulk of quality measures in an ACO contract, but multiple other measures can take place or be scheduled during that visit. Preventive cancer screening, body-mass index measurement, and depression screening are among a few of the individual measures providers can cover in the annual wellness visit.
“A rising tide raises all boats, so if you do an annual wellness visit as it’s supposed to be done, you’re addressing 90 percent of the metrics that need to be captured,” Camacho maintained. “Getting that done in and of itself is huge.”
These visits are largely intended to educate patients around important preventive care practices and healthy lifestyles.
Annual wellness visits can also be used point patients to different, less expensive, sites of care, Nuckolls noted.
“The true North measure is having annual wellness visits,” agreed Nuckolls.
Using High-Quality Data to Inform Decisions
There are two critical ways data informs ACO decision-making: quality metrics and costs of care.
ACO leaders often show providers data on the quality and costs of their own care as well as the care of their peers. This information helps providers identify when they are referring patients to high-cost specialty providers.
“They’ll start shifting referral patterns and work with higher quality, higher performing positions based on the data that we’re applying,” said Camacho. “At the end of the day, the patient is going to get the best care because of what’s happening in the background.”
A lot of this information comes from payers in the form of claims data.
“We use insurance company-provided data, which might be who’s in the hospital right now, who went to the hospital in the last 24 hours, who’s been there in the last week,” McGookin said. “Claims data also shows us what charges are incurred by patients, so we understand where money is being spent and what it is being spent on.”

Michael Camacho, MPA, CHI St. Luke’s Health
Source: CHI St. Luke’s HealthAccess to this data makes it very easy to identify duplicative and wasteful costs. But providers must be educated on how to interpret these data points.
CHI St. Luke’s conducted over 300 visits with physicians to walk them through the data and reporting measures, highlighting what they did well and where they could improve. But Camacho recognized that this method was not sustainable.
“It’s really just shining a light on the issue. We make sure to provide clinicians the technology, the infrastructure, and care management they need. If they need pharmacists to help review some of the meds, we’re going to provide them,” Camacho explained. “ACOs can be kind of this foggy concept and making the numbers of the data real and actionable was crucial.”
Many healthcare organizations still rely on spreadsheets and paper reports to translate data into actionable insights. But a spreadsheet can be overwhelming and difficult to interpret, so many ACOs are investing in point-of-care dashboards.
Through EHR integration, a point-of-care dashboard highlights key quality metrics. Providers opening the EHR during an annual wellness visit can immediately see which gaps in care they should focus on closing for patients based on the ACOs standard of care. The specific metrics are highlighted in the dashboard are largely the result of the ACO agreement between payers and providers.
“We invested in a point-of-care dashboard because we are really trying to focus on gaps in care,” Nuckolls explained.
Quality measures required for payment are almost guaranteed to be on the dashboard because they are linked to payment. But ACOs can add other measures to the dashboard based on their specific patient population’s needs.
“At the end of the day, the patient is going to get the best care because of what’s happening in the background.”
For example, Medicare removed eye exams for patients with diabetes from their reimbursement model, but Coastal Carolina Quality Care kept this metric on their dashboard because it a best practice, Nuckolls explained.
Participating in an ACO does require significant investments, but the model is worth it for organizations like Coastal Medical, CHI St. Luke’s, and Coastal Carolina Quality Care, Inc. Leaders from the three organizations agreed that the ACO model aligns with the future of healthcare, and when providers can participate successfully patients and the practice win.
“It has transformed, guided, and informed how we set up our systems and to a certain extent, how we operate and think about things,” Nuckolls said. “When most of our contracts were fee-for-service, we made sure that we focused on policies, procedures, and operations around the efficiency of the fee-for-service world and you didn’t think as much about the value-based world.”
Now that most of his patients are covered through value-based contracts, Nuckolls and his team are focusing more on improving patient care through comprehensive services like extended access to care, robust care teams, annual wellness visits, and data-driven care.
These services and capabilities are resulting in greater value-based revenue, patient satisfaction, and overall better outcomes for all.
