CMS Timelines for Stage 3 Meaningful Use, MACRA Implementation
CMS developed timelines for Stage 3 Meaningful Use and MACRA implementation that spell out healthcare payment incentives and penalties.

Source: ThinkStock
- For Medicare providers, CMS has set the pace for quality improvements and healthcare payment reform through Stage 3 Meaningful Use and the Quality Payment Program (under MACRA implementation). The programs are designed to put providers on track to achieve healthcare reform and innovation by applying payment incentives or penalties associated with program participation.
Providers should be aware of program timelines to either maximize financial incentives or avoid negative Medicare reimbursement reductions. In the following sections, we will explore CMS timelines and payment schedules for Stage 3 Meaningful Use of the EHR Incentive Programs as well as the Quality Payment Program under MACRA.
Understanding the Value-Based Reimbursement Model Landscape
CMS Payment Reforms Mean Big Bucks for Medicare, Medicaid
Stage 3 Meaningful Use in 2015 and Beyond
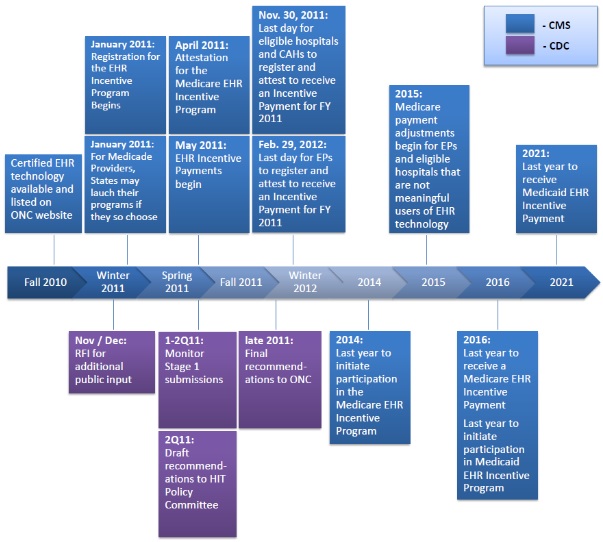
In October 2015, CMS released the final rule for Stage 3 Meaningful Use requirements used to determine if eligible providers would receive incentive payments or negative payment adjustments. Starting in 2016, eligible professionals and hospitals having failed to adopt and demonstrate meaningful use of certified EHR technology (and related health IT) in the preceding year were hit with Medicare payment reductions.
The rule detailed how eligible professionals and hospitals could gradually progress through the three stages of the EHR Incentive Programs until they can “provide efficiencies in administrative processes which support clinical effectiveness, leveraging automated patient safety checks, supporting clinical decision making, enabling wider access to health information for patients, and allowing for dynamic communication between providers.”
Source: Centers for Disease Control and Prevention (CDC)
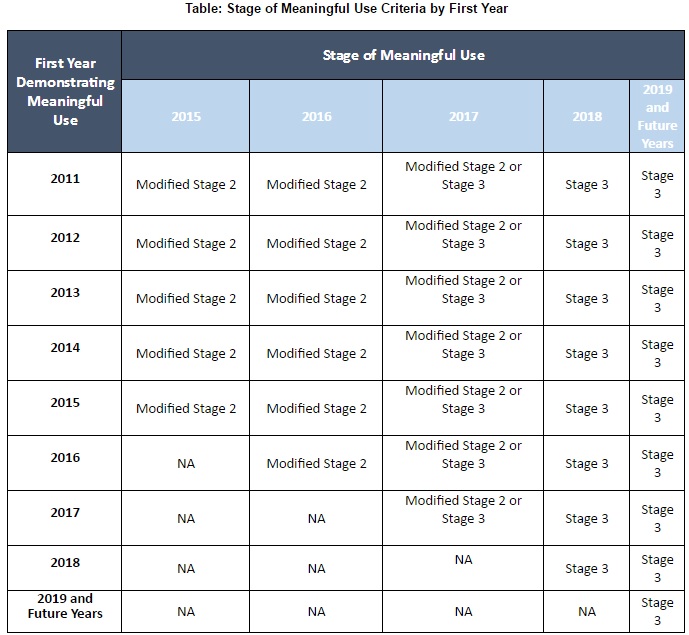
To ease eligible professionals and hospitals into the final stage of meaningful use, CMS developed a modified form of Stage 2 which established a transition period between 2015 and 2017. The final rule combined aspects of Stage 1 and Stage 2 to allow providers to meet a single set of meaningful use requirements for up to three years rather than attest to two separate stages.
According to the modifications, eligible providers must attest to ten objectives (nine for eligible hospitals and critical access hospitals) as well as one consolidated public health reporting measure.
In 2015, eligible professionals in modified Stage 2 were allowed to report on objectives for any continuous 90-day period. However, participants were required to report for the full year starting in 2016, CMS noted, to ensure that providers were significantly moving to Stage 3.
After the transition period, CMS expects all eligible professionals and hospitals to start attesting to Stage 3 Meaningful Use — although providers who elect to participate in 2017 will only have to demonstrate meaningful use for a 90-day period. With the creation of the Quality Payment Program following the publishing of the Stage 3 rule, eligible professionals are exempt from the EHR Incentive Programs beginning in 2017.
Source: CMS
By 2018 and beyond, eligible hospitals will be required to report on Stage 3 objectives for the entire calendar year. The federal agency stated that the Stage 3 objectives and measures “include increased thresholds, advanced use of health information exchange functionality, and an overall focus on continuous quality improvement.”
Participants must attest to eight objectives with related measures to meet Stage 3 Meaningful Use requirements. Some of the objectives are electronic patient health information protection, clinical decision support intervention implementation, robust electronic prescribing use, patient access to health data, and care coordination through patient engagement. Participants will also be required to participate in public health reporting.
CMS reported that more than 60 percent of Stage 3 objectives require health IT interoperability, which is up from 33 percent of Stage 2 objectives. Additionally, the Stage 3 rule aligns clinical quality measure reporting with other CMS-run quality reporting programs and advocates the use of application program interfaces (API) to boost interoperability.
Meaningful use is key to achieving the Office of the National Coordinator’s (ONC) goal of nationwide healthcare interoperability by 2024. The federal agency released its interoperability roadmap in 2015, setting explicit goals for healthcare data sharing.
Top 3 Most Challenging Stage 3 Meaningful Use Requirements
How Does Meaningful Use Impact Revenue Cycle Management?
MACRA Implementation Schedule to Start in 2017
In January 2015, the Department of Health & Human Services (HHS) set a goal of connecting 90 percent of traditional Medicare payments to quality or value by the end of 2018. About half of Medicare payments are also expected to be made under an alternative payment model by the same time. Through the implementation of the Medicare Access and CHIP Reauthorization Act (MACRA), the federal agency's value-based goals may come to fruition.
In April, CMS proposed a MACRA implementation rule that would establish the Quality Payment Program, which would start linking Medicare payments to value by 2017. Under the Quality Payment Program, eligible clinicians — formerly eligible professionals under meaningful use — will participate in either the Merit-based Incentive Payment System (MIPS) or in an Advanced Alternative Payment Model (APM). Most Medicare clinicians, CMS explained, are likely to start in MIPS, which consolidates and streamlines several value-based and quality improvement programs, including the Physician Quality Reporting System, Value-based Modifier Program, and EHR Incentive programs.
According to the proposed rule, the first MIPS performance year would start on January 1, 2017, bringing an end to the other quality reporting programs by the close of the 2016. Performance during 2017 will determine Medicare Part B payment adjustments in 2019.
CMS plans to limit the 2019 payment adjustments to no more than four percent upward or downward, but the adjustments would increase over time. The federal agency proposed a five percent maximum adjustment in 2020 that would increase to nine percent by 2022.

Source: CMS
Medicare reimbursement adjustments would be calculated based on MIPS composite performance scores. The score is made up of four performance categories: quality, advancing care information, clinical practice improvement activities, and cost.
In the 2017 performance year, care quality performance will account for 50 percent of the total MIPS score. Eligible clinicians would report on six out of 200 measures, including one cross-cutting and one outcome measure or another high-quality measure.
The advancing care information component would represent 25 percent of the MIPS composite score in 2017. For this category, eligible clinicians would have to demonstrate EHR use by reporting on six objectives similar to those in the Meaningful Use program. Points would also be awarded for EHR use performance and additional public health reporting.
Another 15 percent of the MIPS score would reflect Clinical Practice Improvement Activities, such as approved care coordination, patient engagement, and patient safety improvement initiatives. CMS proposed over 90 approved activities and the federal agency would weigh the activities based on level of difficulty.
The final ten percent of the MIPS score would represent an eligible clinician’s healthcare costs. Using Medicare claims, CMS would calculate an average score based on 40 episode-specific measures. However, if eligible clinicians do not have sufficient patient volumes for any cost measures, CMS would not determine a cost score and adjust the other MIPS category scores.
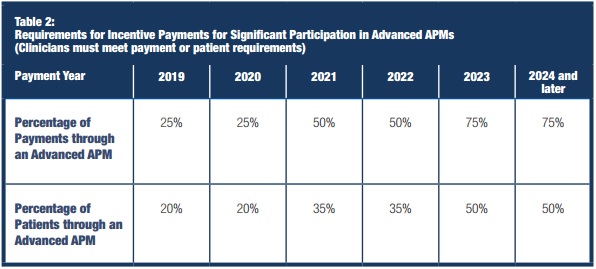
Under the Advanced APM track, eligible clinicians can participate in an approved alternative payment model in 2017, such as the Comprehensive Primary Care Plus initiative, Medicare Shared Savings Program Tracks 2 and 3, and the Next Generation accountable care organization model. Advanced APM participants between 2019 and 2024 may qualify for a five percent Medicare Part B incentive payment in lieu of MIPS payment adjustments.
By 2026, however, CMS proposed that Advanced APM participants would receive a higher fee schedule update rather than an incentive payment. Participants will also be excluded from MIPS participation.
CMS also intends to add more requirements to the Advanced APM track. For the first performance year, Advanced APM clinicians must have at least 25 percent of Medicare payments and 20 percent of Medicare patients under the alternative payment model. The federal agency would increase the thresholds to 50 percent of Medicare payments and 35 percent of Medicare patients by 2021, then 75 percent of Medicare payments and 50 percent of Medicare patients by 2023.
Source: CMS
The participation thresholds may also include non-Medicare reimbursements and patients by 2021 depending on the final MACRA implementation rule, CMS noted.
Additionally, CMS announced in September that eligible clinicians will have more options for MACRA attestation in 2017. The federal agency offered four levels of participation for the first performance year, ranging from just testing the Quality Payment Program to fully participating in an Advanced APM.
The first three options allow eligible clinicians to choose how much data they submit to the program and for how long. Eligible clinicians must submit at least some data to avoid a negative payment adjustment, while reporting for part of the performance year would qualify participants for a “small” positive payment adjustment and reporting for the full year would qualify clinicians for a “modest” positive payment adjustment.
Eligible clinicians who select the Advanced APM option would still qualify for the five percent incentive payment in 2019.
What We Know About Value-Based Care Under MACRA, MIPS, APMs
How MACRA, MIPS Will Impact Critical Access Hospitals, FQHCs
