86% Say Provider Compensation Tied to Fee-for-Service, Salary
Organizations should implement performance-based compensation and data analytics tools to boost value-based care adoption among providers, a new study claims.

- About 86 percent of primary care physicians and specialists reported that their provider compensation was still primarily under fee-for-service or salary arrangements, representing a modest increase from 84 percent in 2014, according to a recent Deloitte Center for Health Solutions survey.

Researchers contended that healthcare organizations can spur value-based care adoption by including more performance-based financial incentives as part of provider compensation and implementing data analytics tools that allow providers to understand healthcare cost and quality performance.
“Physicians should change their behavior to make implementation of value-based care models effective,” stated Mitch Morris, principal at Deloitte Consulting LLP and healthcare industry leader at Deloitte. “But today there is little incentive for them to change; many are still being paid under fee-for-service models and they're not equipped with tools that could help them deliver high-value care.”
While provider compensation was still based on fee-for-service or salary, researchers found that value-based reimbursement increased in the last two years. The survey of 600 providers showed a rise in value-based payment from 25 percent in 2014 to 30 percent in 2016.
However, few providers were under a value-based care model with the greatest downside financial risk. About ten percent reported compensation through capitation and four percent through shared-savings arrangements.
Financial bonuses based on provider performance were also uncommon in 2016. One-half of providers stated that ten percent or less of their compensation was tied to performance bonuses and about 33 percent said they were ineligible for performance bonuses.
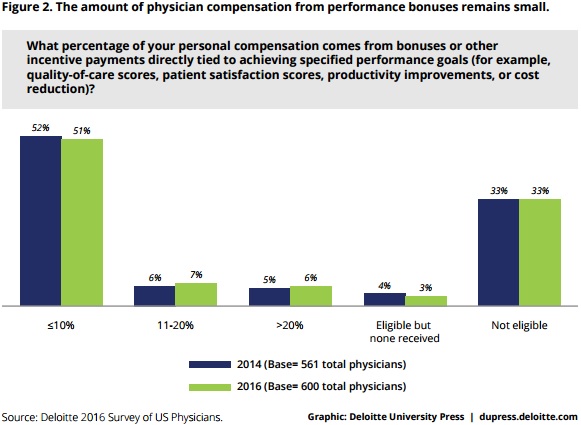
The survey’s findings show that performance- and value-based reimbursement is below the threshold of 20 percent of compensation that healthcare experts have agreed would effectively incentivize providers to change behaviors.
The survey indicated, however, that healthcare organizations may struggle to add more value-based incentives to provider compensation. The top preferred provider compensation arrangements were fee-for-service with 40 percent and salary with 38 percent.
Only 11 percent selected shared savings models as their most preferred compensation arrangement, followed by episode-based payments for specialists with eight percent.
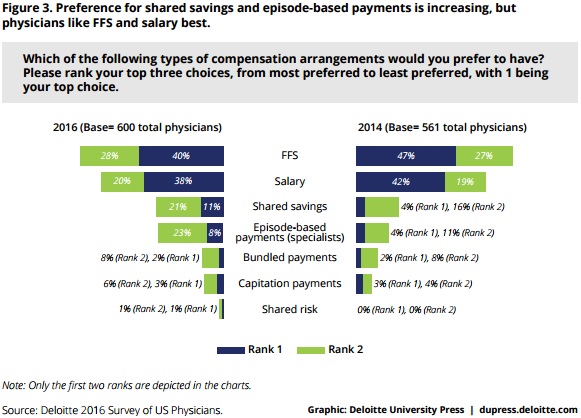
Although, researchers found that some providers were willing to risk a significant portion of their compensation under value-based reimbursement if required to. Researchers found the median reported proportion of provider compensation to be under value-based reimbursement was 15 percent, meaning one-half of providers would put more than 15 percent of compensation at risk and the other half would put less than 15 percent.
Additionally, the survey showed that increased access to data analytics tools that provide clinical decision support and provider performance also can boost value-based care adoption.
Researchers reported that three out of four providers have evidence-based clinical protocols, but only 36 percent have access to comprehensive protocols for many conditions, which are beneficial for improving patient outcomes and standardizing care delivery under value-based reimbursement models.
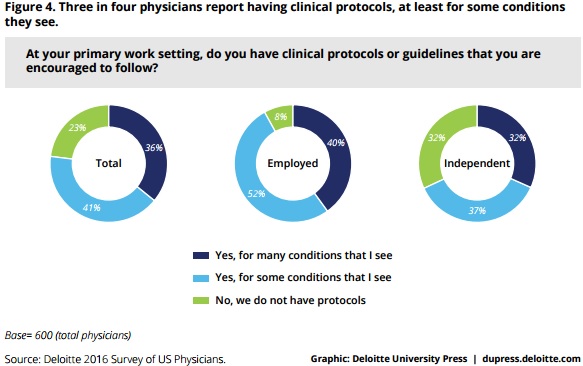
Those who did have clinical protocol access, though, expressed more favorable views about value-based reimbursement models and public reporting of provider performance. Forty percent of providers with clinical protocol access supported value-based reimbursement models compared to 31 percent of those who did not have clinical protocols.
Inpatient-based facilities fared better with protocol availability with 90 percent of providers reporting access versus 69 percent of outpatient-based providers. Employed providers also had greater access to clinical protocols with 92 percent reporting availability compared to just 68 percent of independent providers.
Researchers noted that independent practices may not have high rates of clinical protocol implementation because it requires expensive EHRs and clinical decision supports.
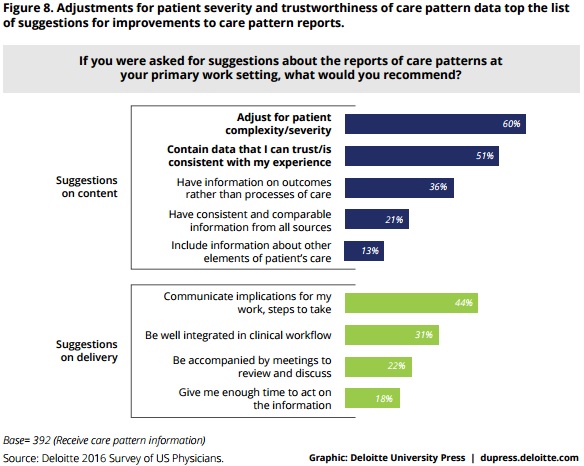
Providers also reported limited access to care pattern reports that provided analysis on clinical outcomes, patient experience, and resource use. About 65 percent of providers stated that they received care pattern information.
However, even if providers received care pattern reports, providers stated that they mostly received information on process measures, such as quality of care measures, instead of clinical outcomes. Thirty-six percent of providers would rather have outcome information over process analysis.
Similarly, the survey indicated that limited healthcare cost and quality data on specialists impeded value-based care success. Providers cited trust or working relationship (75 percent) and specialized expertise (69 percent) as the top reasons for patient referrals, while 15 percent of providers thought of outcomes or quality rating and healthcare costs to patients. Only one percent considered physician fees.
“Given this interest and MIPS incentives tied to resource use measures, physicians may see value in referring patients to providers who routinely use low-intensity (or conservative) approaches,” the report stated. “Additionally, if the current trend of increased patient cost sharing due to high deductibles continues, physician interest in cost-related information may grow, since many physicians are attuned to patient access considerations.”
To encourage value-based care adoption, researchers advised healthcare organizations to connect provider compensation to performance, implement data analytics and decision-support tools, and invest in interoperable health IT.
Organizations should tie at least 20 percent of provider compensation to performance goals, the report stated. Based on survey results, researchers noted that value-based incentives are not enough to motivate providers to change behaviors.
Providers should also have access to data analytics and decision-support systems that are easy to use and understand. The tools should present healthcare data in a meaningful and appropriate way for providers to use during care delivery.
“Physicians desire a broadening of available clinical protocols, quality measures that align with their specialties and emphasize outcomes rather than processes of care, and detailed data on their own performance and on those to whom they refer patients,” the report added. “Our survey findings suggest that many physicians currently lack these tools, but when made available, they impact performance.”
Lastly, healthcare organizations should invest in technology capabilities that promote interoperability and integration of health IT. Providers in the survey expressed distrust with the data they received or stated that they could not integrate it into their daily practices.
More advanced health IT capabilities would help providers access timely, reliable, and actionable information. With this data, providers could understand benchmarks and incorporate value-based care goals into their workflows.
Image Credit: Deloitte Center for Health Solutions
Dig Deeper:
• Understanding the Value-Based Reimbursement Model Landscape
• Physician Compensation Models Need Value-Based Reimbursement
