88% Improve Claims Submissions Using Revenue Cycle Analytics
A recent survey found that a majority of healthcare organizations using revenue cycle analytics were able to improve key performance indicators, including claims submissions.

- According to a Navicure survey, medical organizations that used a revenue cycle analytics or business intelligence solution were able to boost performance on key healthcare revenue cycle metrics.

About 88 percent of participants reported that claims submissions improved, followed by rejection rates (84 percent), denials (78 percent), cash flow (76 percent), and patient billing and payments (66 percent).
“Now more than ever, healthcare organizations are realizing the benefits of implementing a robust data analytics and reporting program,” said Jim Denny, CEO of Navicure. “As organizations are tasked to further improve and report value, this research confirms data analytics and reporting solutions will play an increasingly important role.”
The respondents stated that revenue cycle analytics programs were able to help their healthcare organizations streamline cash flows and identify problem areas.
Seventy-one percent of participants reported that their organizations improved cash flows by reducing days in accounts receivable.
A little over half of the respondents found that their facilities increased revenue by using a solution to identify bottlenecks to getting paid, while 48 percent stated that the solution helped boost staff productivity by pinpointing areas for additional training.
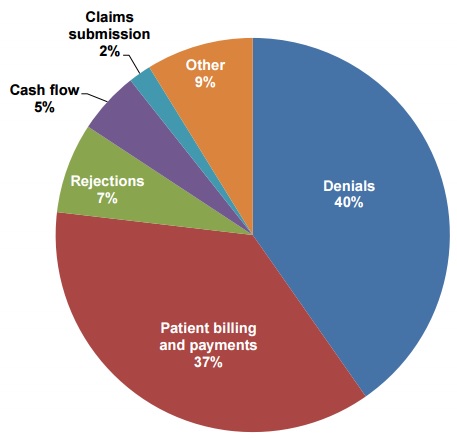
Healthcare organizations also used revenue cycle analytics programs to target the top challenges to revenue cycle management, explained the survey.
Participants stated that the most significant difficulties with managing healthcare revenue cycles were reducing days in accounts receivable and lowering denial and rejection rates (55 percent). Over one-third rated patient billing and payments as the second most significant challenge.
Notably, the solution helped to actively manage claims denials, which 40 percent of respondents listed as the top healthcare revenue cycle challenge.
Despite some success with revenue cycle and business intelligence analytics programs, 55 percent of healthcare organizations did not have a data analytics and reporting solution to improve their revenue cycle.
However, the survey explained that the demand for these solutions is increasing as more providers transition to value-based care. Almost half of the respondents are currently searching for a revenue cycle analytics program.
Eighty-eight percent also reported that analytics and business intelligence solutions are extremely or very important for making business decisions.
Additionally, researchers found that a majority of leadership teams view acquiring revenue cycle analytics and business intelligence programs as a high priority.
The survey explained that using a revenue cycle analytics system could help healthcare organizations stay financially healthy while their providers focus on improving patient and cost outcomes.
Many of these solutions can help to streamline value-based care reporting for some key performance indicators, such as denial and rejection rates, patient and payer payment trends, charge lags, and first pass rates, the survey stated.
Researchers advised healthcare organizations to seek revenue cycle analytics solutions that possess the following capabilities:
• Claim monitoring activities from submission to post-adjudication, including how long it takes to get paid
• Dashboards that show important key performance indicators
• Reports that identify the root-cause of claim issues
• Benchmarks for comparative analysis
• Robust reporting abilities.
“Implementing a user-friendly solution that streamlines reporting with actionable data will facilitate informed decision making and ongoing revenue cycle improvements, helping organizations achieve greater financial health and position them for future success,” added Denny.
While managing the transition to value-based care is difficult for many healthcare organizations, it can be especially challenging when some payments are still tied to fee-for-service structures. Some systems from the fee-for-service world may not be equipped to handle the data-driven models of value-based care.
Image Credit: Navicure
Dig Deeper:
• Using Revenue Cycle Analytics for Effective Value-Based Care
• Preparing the Healthcare Revenue Cycle for Value-Based Care
