Declining Accountable Care Organizations Represent Expansion

The dawn of 2015 for the healthcare industry began with the Centers for Medicare & Medicaid Services (CMS) announcing an additional 89 provider organizations enrolling in the Medicare Shared Savings Program (MSSP) as accountable care organizations (ACOs).
ACOs — groups of doctors, hospitals, and other healthcare providers that collectively coordinate efforts to provide Medicare beneficiaries in fee-for-service quality coordinated care — can share in any Medicare generated savings if they meet specified identified quality objectives. Healthcare providers acknowledge responsibility for a distinct population’s cost and quality of care.
The implementation of a trifold objective within the healthcare industry means changing how providers are paid by focusing on effectively meeting specific cost and quality benchmarks, says Donald Berwick, President Emeritus and Senior Fellow at the Institute for Healthcare Improvement, et al.
“Improving the U.S. health care system requires simultaneous pursuit of three aims: improving the experience of care, improving the health of populations, and reducing per capita costs of health care,” explains Berwick.
CMS acknowledged that when provider organizations join the MSSP as ACOs, this is merely one facet of a continued vision to advance the coordinated management and assimilated integration of care Medicare beneficiaries receive.
Recent numbers represent a reduction in new entrants in comparison with those previously reported within the last several years. 2014 began with CMS announcing one hundred and twenty three new MSSP ACOs. 2013 began with CMS announcing one hundred and six new MSSP ACOS.
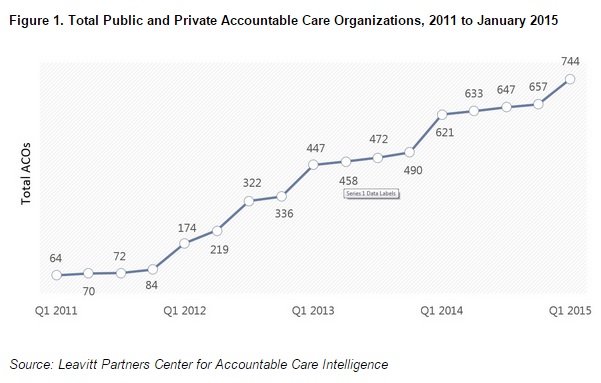
While this year’s new entrants are a smaller cohort than those that joined in 2013 and 2014, they represent a continuation of the expansion of the accountable care movement,” says David Muhlestein, PhD, Director of Research at Leavitt Partners.
“There is strong support for this care delivery approach to continue,” says Muhlestein.
The government actively supports and endorses transitioning half of Medicare payments to alternative payment models, including ACO-based arrangements, as states seek to control the Medicaid costs.
“In 2014 alone, existing Shared Savings Program ACOs added almost 17,000 healthcare providers, and the 89 new ACOs will bring approximately 23,000 additional physicians and other providers into the ACO program starting January 1,” says CMS. “The growth of this program for providing health care has been continued and consistent since its inception, and we are encouraged by that interest.”
Since ACOs first started to participate in early 2012, thousands of healthcare providers now participate in the program to collectively provide improved care to Medicare’s seniors and people with disabilities, says CMS.
As RevCycleIntelligence wrote last month, it is expected that thirty percent of traditional, fee-for-service Medicare payments will transition into value-based payments via alternative payment models by the end of 2016. This number includes ACOs. HHS additionally proposed to shift eighty-five percent of traditional fee-for-service Medicare payments to quality of value within the next year.
According to active ACO tracking conducted since 2010, one hundred and twenty organizations have become ACOs in both public and private programs. This brings the total number of organizations since 2011 to seven hundred and forty-four.
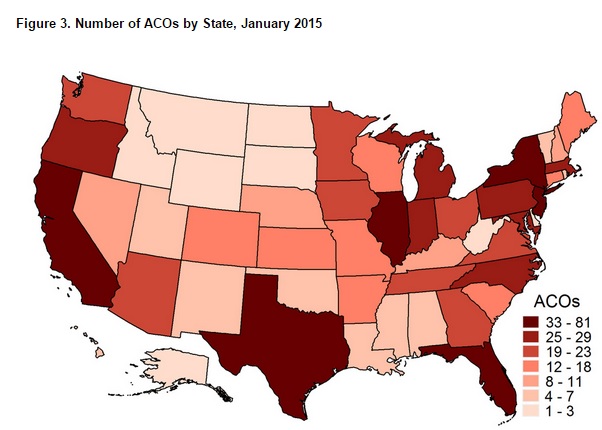
According to a Muhlestein’s Leavitt Partners report, while only nine states do not have ACOs, less than half of all three hundred and six Hospital Referral Regions (HRRs) have an ACO.
“This clustering within HRRs suggests that competing health systems are simultaneously creating ACOs,” the report confirms. “This may arise from providers in a market who seek to match or copy what a competitor is doing or it may be indicative of previously-integrated systems that are better prepared to become ACOs.”
The report confirms a clear trend toward hospital systems sponsoring ACO development since they accounted for over sixty percent of all sponsoring entities.
Muhlestein says the growth in the total number of ACOs and the associated number of covered lives is only part of the story. Overall, there are over one thousand known contracts for seven hundred and forty four ACOs, he adds.
As the growth of the accountable care movement continues, 2015 will be a deciding year as to whether the ACO model will effectively make the shift from a series of exploratory programs toward mainstream nationwide adoption, says Muhlestein.
Although becoming an ACO involves significant time and resources, such research may hopefully predict the success of ACOs within the future direction of the healthcare industry as progression into value-based and consumer-centric care approaches moving closer into the new dawn of ICD-10 implementation.
