Few Docs Familiar with MACRA, Transitioning to Value-Based Care
A new survey indicates that physicians are not engaged enough with value-based reimbursement models, such as MACRA, to achieve the Triple Aim.

- Only 20 percent of physicians reported that they are very or somewhat familiar with MACRA, according to a recent survey from the Physicians Foundation and Merritt Hawkins, and the majority of respondents do not currently have a large portion of their reimbursements time to value-based models.

Researchers found that 79 percent or more of physician compensation was still under a fee-for-service model in 2016, indicating that value-based reimbursement models are not gaining traction with providers despite upcoming Medicare changes like MACRA.
Unfamiliarity with the value-based reimbursement program is one example of how providers are not buying into healthcare payment reforms designed to transition to value-based reimbursement models, the survey of over 17,000 physicians suggests.
“As a central player in determining patient treatments and care plans, physician participation and leadership is critical to transforming healthcare from a system driven by the volume of services to one focused on the value of services,” stated an accompanying press release. “However, the survey indicates that the majority of physicians are not convinced to sufficiently engage or support the mechanisms of healthcare reform to achieve its stated aims.”
Although HHS announced earlier this year that it has met its goal of linking 30 percent of Medicare payments to quality and value, about 18 percent said their practice did not tie 30 percent of reimbursements to value, while half (50.3 percent) stated that they were unsure.
The low volume of value-based payments and uncertainty surrounding value-based care models translated to low alternative payment model participation in 2016, the survey showed. When asked if any of their reimbursements were connected to value or quality-based metrics, such as patient satisfaction and treatment protocols adherence, 45.1 percent said no, 42.8 percent responded yes, and 12.1 percent were unsure.
“The fact that over 12% of all respondents are unsure whether they receive value-based payments underscores the continued novelty of these payment models in the eyes of many physicians,” stated the survey.
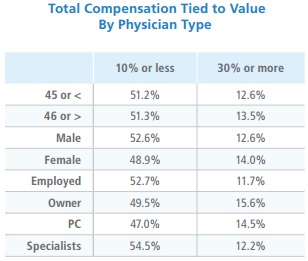
Even among the providers who responded yes to value-based payments, the proportion of reimbursements tied to value or quality was still low, especially compared to the HHS goal. The majority (51.3 percent) noted that 10 percent or less of their total payments were linked to value, while only 13.1 percent had 30 percent of total payments tied to value.
While some providers participated in a range of value-based reimbursement models, including medical homes and bundled payments, physicians were especially concerned about how accountable care organizations (ACOs) would improve their practices. Nearly 39 percent of physicians believed that ACOs were unlikely to enhance quality of care or reduce healthcare costs, which is up from 36.3 percent in the 2014 survey.
The survey explained that ACOs have been operating longer than some other value-based reimbursement models and cover between 15 percent and 17 percent of the population, but many physicians are still unsure about ACO functions. Nearly 28 percent of physicians were uncertain about the structure and purpose of ACOs.
However, the proportion of physicians unfamiliar with ACO structures has modestly decreased since the previous two surveys. About 32 percent reported uncertainty about ACO functions in 2014 and 28.6 percent said the same in 2012.
“Implementation of the ACO models depends on physician understanding and integration,” stated the survey. “The 2016 survey suggests that these goals have yet to be achieved and that physician integration will continue to be a challenge for those charged with ACO implementation.”
The poll also showed that other healthcare reforms, such as ICD-10 and EHR use, have yet to provide physicians with evidence of care delivery and revenue cycle enhancements. While ICD-10 was implemented in October 2015 to boost physician efficiency, improve billing precision, and enhance patient care, the survey reported that most providers have not realized these benefits from the system.
Only 5.8 percent of physicians stated that ICD-10 improved practice efficiency, while six percent said the system boosted revenues and five percent said it enhanced patient care. Most providers reported that ICD-10 has had little to no impact on the three areas, whereas one-quarter or more said it detracted from the areas.
Physician perspectives on EHR technology were similarly tepid, according to the survey. Only 29 percent reported that EHRs improved quality of care, 25.3 percent said it boosted efficiency, and around 11 percent stated it enhanced patient interaction.
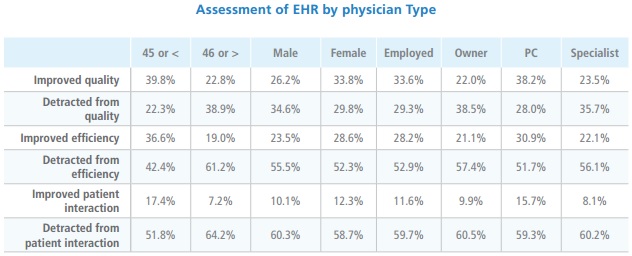
The 2014 survey reported that 47.1 percent of physicians said that EHRs detracted from patient interaction, but that number jumped to 59.8 percent in 2016.
Despite many physicians expressing unfamiliarity or negative views of recent healthcare reforms, the survey found that employed providers were more likely to understand and participate in value-based reimbursement models.
“[T]he employed model promotes the system integration necessary to implement fee-for-value payments, and it is therefore unsurprising that a considerably greater number of employed physicians indicate they receive value-based payments than do practice owners,” reported the survey.
The number of employed physicians also grew in 2016 as more healthcare reforms were implemented, the survey stated. About 44 percent of physicians identified as hospital or medical group employees in the 2012 survey, but the proportion increased to nearly 53 percent in 2014 and almost 58 percent in 2016.
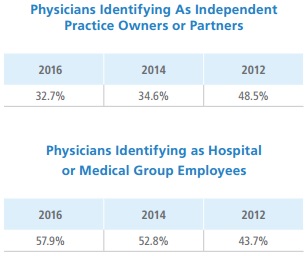
Physicians are moving away from private practices to larger facilities to better manage the changing healthcare landscape.
“Employment provides the security of an assured income at a time when physician reimbursement models are in flux and private practice physicians are unsure of how they will be paid or whether they can cover private practice expenses,” the survey stated. “Employment also is thought to lessen the regulatory and compliance burden private practice physicians face, while providing them with the financial support and technical expertise needed to implement mandated use of information technology.”
However, only half (49.9 percent) of surveyed physicians agreed that hospital employment is a positive trend. Increases in employed physicians could lead to “a loss of clinical and administrative autonomy,” the survey stated. The unenthusiastic views on hospital employment may also contribute to the lack of support behind value-based reimbursement models.
“The survey strongly indicates that considerably more physician support and participation will be required to achieve the goals of healthcare reform and to transform the healthcare system from one based on volume to one based on value,” concluded the survey.
Image Credit: The Physicians Foundation
Dig Deeper:
• Understanding the Value-Based Reimbursement Model Landscape
• What We Know About Value-Based Care Under MACRA, MIPS, APMs
