Fewer Hospitalizations Reduced Skilled Nursing Facility Use by 15%
Skilled nursing facility use declined since 2009 as hospitals reduced their inpatient costs under value-based reimbursement models, an analysis showed.
Source: Thinkstock
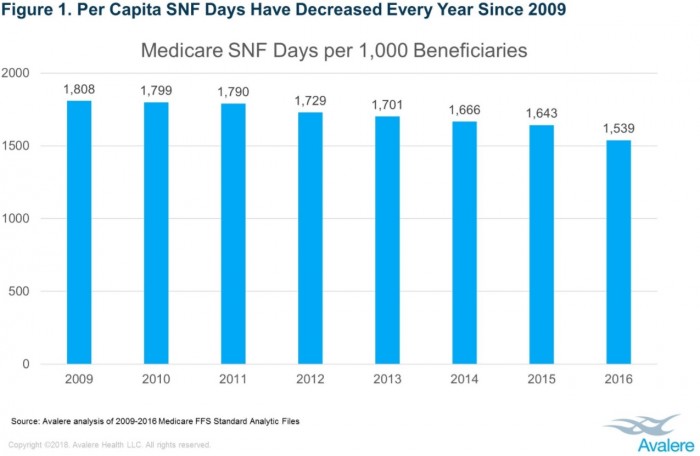
- Skilled nursing facility (SNF) utilization has declined 15 percent from 2009 to 2016, a new Avalere analysis revealed.
The analysis of Medicare fee-for-service claims revealed that SNF utilization dropped from 1,808 SNF days per 1,000 Medicare fee-for-service beneficiaries to just 1,539 days in 2016.
Source: Avalere
“The economics of post-acute care have been fundamentally changed as Medicare shifts its payment approach to capitation, bundles, and pay-for-value,” stated Dan Mendelson, Avalere’s President. “Fewer patients are being admitted to the hospital, as payers and risk-bearing providers seek to shift care to lower-cost settings.”
As Mendelson pointed out, hospitalization rates contributed to a drop in SNF use, not necessarily a shift in how hospitals use post-acute care facilities as some stakeholders argue.
The shift away from fee-for-service is prompting hospital providers and leaders to reconsider inpatient admissions. Value-based reimbursement models hold hospitals accountable for the total costs of care for patients, and hospitalizations can quickly run up an organization’s costs.
Inpatient hospital costs totaled $381.4 billion in 2013, with the mean expense per stay reaching $18,000, the Healthcare Cost and Utilization projected reported.
With inpatient stays emerging as a cost-cutting opportunity, hospitals are trying to ensure that only patients who truly need an inpatient stay are occupying hospital beds.
Post-acute care can also impact a hospital’s bottom line under value-based reimbursement models. Hospitals are responsible for the financial and clinical outcomes of patients even after they are discharged under bundled payments, capitation, and other alternative payment models.
Ensuring providers discharge patients to the appropriate, low-cost post-acute care facility is key to reducing total costs of care and improving patient outcomes. A heavy emphasis has been placed on safely discharging patients to their homes if possible because it is the lowest cost setting.
However, the Avalere analysis showed that a decline in hospitalizations is driving the reduced use of skilled nursing facilities, rather than a shift in post-acute care use.
Low hospitalization rates may spell trouble for skilled nursing facilities. Medicare covers up to 100 days of SNF care for patients discharged from an inpatient stay. However, a patient must have an inpatient stay lasting at least three days to qualify for coverage.
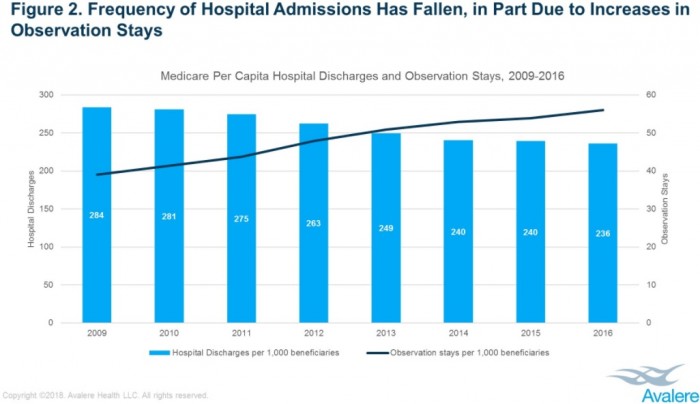
As hospitalizations decrease, patients qualifying for Medicare coverage of SNF care also declines. Per capita hospital discharges fell 17 percent since 2009, the analysis from Avalere showed.
Conversely, the number of hospital observation stays increased during the study’s period.
Source: Avalere
Hospitals use observation stays to keep low-acuity patients under provider care without the inpatient admission. As hospitals enter value-based reimbursement arrangements that penalize for excessive readmissions and face new inpatient reimbursement rules, such as the Two-Midnight Rule, observation stays have emerged as an alternative to the expensive inpatient stay.
Additionally, researchers did not observe significant shifts in post-acute care use by hospitals between 2009 and 2016. The proportion of discharges to SNFs versus home health agencies, inpatient rehabilitation facilities, and long-term acute care hospitals did not significantly change from 2009 to 2016.
The average length of stay at SNFs also did not substantially change. The average SNF length of stay remained at about 24 days between 2009 and 2016, the analysis revealed.
“The long-term erosion in hospitalizations contributes directly to the decline in skilled nursing facility utilization among Medicare beneficiaries,” explained Fred Bentley, Vice President of Avalere Health. “While hospitals that are aggressively moving to value-based payment are shifting discharges from skilled nursing facilities to home health providers, the biggest driver of the decline in skilled nursing facility use appears to be the reduction in hospitalizations.”
