Hospitals Could Lose Up to $4.1B Under Medicaid Work Requirements
Medicaid work requirements would harm hospital finances, reducing revenue and boosting uncompensated care costs by $2.5 billion to $3.7 billion in 2019.

Source: Thinkstock
- Medicaid work requirements would reduce hospital revenue between $3.7 billion to $4.1 billion in 2019 alone, according to a recent analysis by the Commonwealth Fund.
Hospitals in over a dozen states considering Medicaid work requirements would also face higher uncompensated care costs, totaling between $2.5 billion and $3.7 billion in 2019, the non-profit private foundation found using a hospital simulation model.
“At a time when many rural hospitals throughout the nation have shuttered, the move to impose work requirements on Medicaid beneficiaries ultimately weakens hospitals. Because hospitals are often a major economic engine in a community, these work requirements can hurt the entire local economy,” stated report author Allen Dobson, PhD, Cofounder and President of Dobson DaVanzo & Associates LLC.
Dobson, DaVanzo conducted the analysis for Commonwealth Fund, which extrapolates the early results of Medicaid coverage loss from the implementation of Medicaid work requirements in Arkansas and other recent studies that estimate the financial impact of work requirements.
Arkansas was the first state to implement work requirements in Medicaid. The state launched the program in June 2018, targeting enrollees between 30 and 49 years old and expanding the population to individuals between 19 and 29 years old in January 2019.
READ MORE: The Difference Between Medicare and Medicaid Reimbursement
Early results show nearly 8,500 individuals lost Medicaid coverage within the first four months of the program, and between 23 and 29 percent of the targeted population either did not meet the work requirement or failed to report their work activities each month, which could result in lost coverage.
Similar reductions in Medicaid coverage would also impact the 14 other states imposing or looking to impose Medicaid work requirements. But how the programs will impact hospital finances depends on the design of the work requirements, the analysis showed.
For example, hospitals in states that apply work requirements to both traditional Medicaid and Medicaid expansion beneficiaries would see the greatest reduction in revenue, the analysis showed.
Researchers projected Medicaid revenue to decline by 18 to 20 percent on average in Indiana and 20 to 22 percent in Kentucky. Both are Medicaid expansion states and have CMS approval to apply Medicaid work requirements to expansion and traditional adults up to age 59 and 64, respectively.
In contrast, Medicaid revenue for states like Arizona, Arkansas, and Ohio, which only apply work requirements to the Medicaid expansion population up to age 49 would fall by 10 to 14 percent.
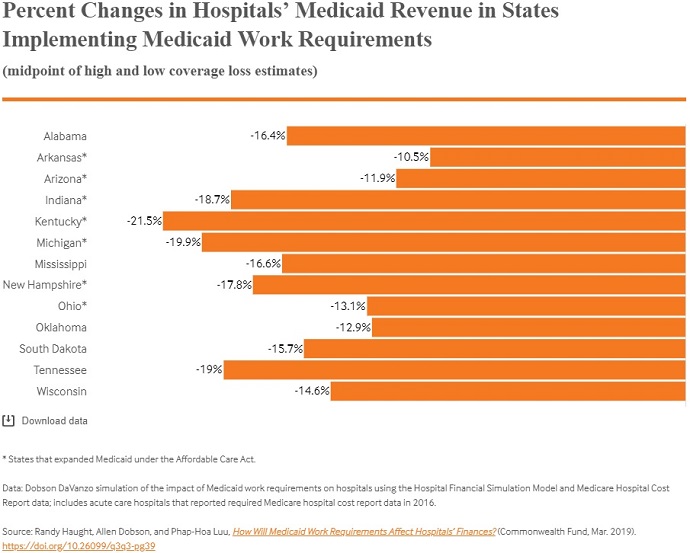
Source: Commonwealth Fund
READ MORE: How the Affordable Care Act Impacted Healthcare Revenue Cycle
States that apply work requirements to both populations could also see the greatest increase in uncompensated care costs, the analysis revealed.
Hospitals in Kentucky would experience the largest increase in uncompensated care costs. Researchers estimated that the hospitals would see a 133.7 percent increase in uncompensated care costs under the work requirement program that applies to traditional and expansion populations.
Additionally, hospitals in expansion states would see large uncompensated care growth due to coverage losses.
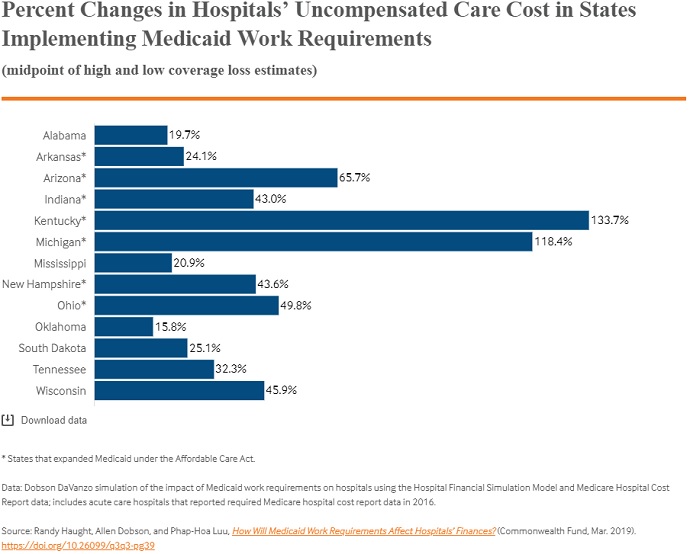
Source: Commonwealth Fund
With revenue falling and uncompensated care costs rising, hospital operating margins would take a hit under Medicaid work requirement programs. Operating margins, which measure hospital profitability on the income or losses from patient care, would fall between 0.4 and 2.2 percent across the 15 states.
But again, the impact on hospital operating margins would also vary across the states. Hospital payer mix, the portion of Medicaid enrollees subject to work requirements, the number of individuals that lose coverage, and the portion of Medicaid beneficiaries that become uninsured all impact the effect on hospital operating margins.
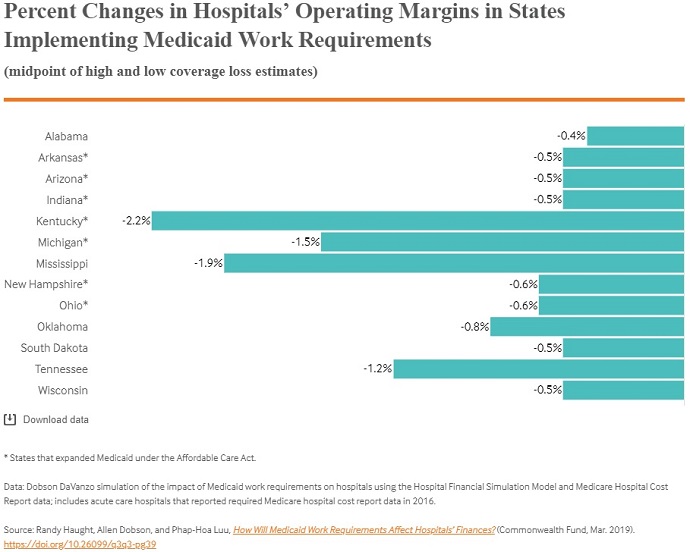
Source: Commonwealth Fund
READ MORE: Finding Medicaid Eligibility Cuts Hospital Bad Debt by 10%
Kentucky hospitals, for example, would see the greatest decline in operating margins (-2.2 percent) because the program applies work requirements to traditional and expansion beneficiaries up to age 64.
Rural hospitals would also be hit the hardest by the loss of Medicaid coverage, researchers added.
Most rural hospitals already operate on a deficit, with a recent study showing 41 percent of the facilities operating with negative margins. The coverage losses stemming from work requirement programs would further reduce operating margins, putting more rural hospitals at risk of closing.
Seven states already received approval from CMS to impose Medicaid work requirements and eight states were awaiting approval at the time of the study’s publication. Arkansas is still the only state in which work requirements have been officially implemented, but one of the pending states recently received the green light to start implementing its program.
“Ohio added over 20k jobs in January. With employment steady under 5%, there are great opportunities to connect adults on Medicaid w/ opportunities to improve their lives & health – so I’m pleased to send Governor Mike DeWine the 9th approval of a community engagement waiver,” CMS Administrator Seema Verma states in a tweet announcing the approval of Ohio’s work requirement program.
The Trump Administration is paving the way for Medicaid work requirement programs. The administration issued guidance in January 2018 to help states design demonstration programs.
