Insurance and Medical Billing Costs for Providers Reaches $282B
Insurance and medical billing costs represent a significant portion of provider revenue and about half of those costs are excessive, new research shows.

Source: Thinkstock
- Providers and payers spend about $496 billion on insurance and medical billing costs, with about one-half of the costs being excessive, reveals a new issue brief from the independent policy institute, Center for American Progress.
Providers specifically spent about $282 billion on insurance and medical billing costs, the brief added.
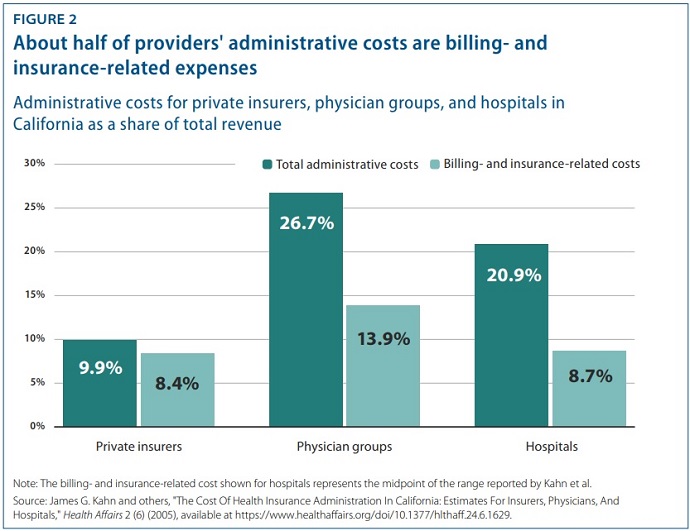
But only about one-half of all provider administrative costs go to billing and insurance, researchers pointed out. Hospitals and physician groups also incur costs for medical record keeping, hospital management, initiatives that track and improve care quality, and more.
“The United States spends much more on administrative costs in healthcare than other developed countries,” Emily Gee, health economist at the Center for American Progress and co-author of the brief, stated in a press release. “This brief details how payment reforms can help rein in these costs for patients and the government.”
Healthcare spending is currently a major issue for policymakers and industry leaders, and administrative costs are at the center of the problem.
READ MORE: Exploring the Fundamentals of Medical Billing and Coding
Federal actuaries project national healthcare spending to increase by 5.5 percent annually until 2027, with healthcare spending on track to exceed 19 percent of GDP by the end of the period. The US already spends about twice as much on healthcare per capita compared to other countries in the Organisation for Economic Co-operation and Development (OECD).
The spending gap is only slated to increase as US healthcare spending rises.
Healthcare administrative costs may be to blame, recent research shows. A 2018 JAMA study comparing US healthcare spending to the rates of similar countries found that administration and governance costs represented eight percent of US GDP compared to a mean of three percent for all countries analyzed.
The study also showed US physicians reported a greater level of administrative burden, with 54 percent saying time spent on administrative tasks related to billing and insurance was a significant problem for them.
Providers are putting a substantial portion of their revenue toward administration, the Center for American Progress report confirmed.
READ MORE: Medical Billing, Patient Access Top Revenue Cycle Risks of 2019
Healthcare administrative costs accounted for nearly 27 percent of total revenue for physician groups and 21 percent for hospitals, the brief stated.
Source: Center for American Progress
Of the administrative share of total revenue, billing and insurance-related expenses represented almost 14 percent and 8.7 percent for physician groups and hospitals, respectively.
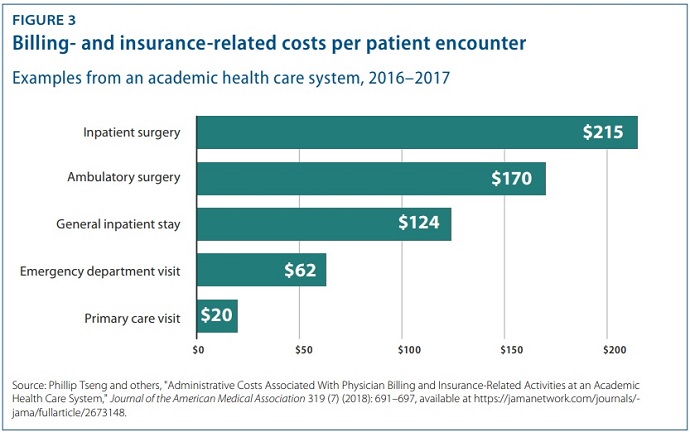
Researchers found that that the type of visit influenced a provider’s administrative costs. Based on the data from a 2018 study of an academic health system by Philip Tseng and others, researchers showed professional billing costs were $20.49 for a primary care visit, $61.54 for an emergency department visits, and $124.26 for a general inpatient stay.
Compared to the professional revenue associated with each type of visit, the emergency department visit generated the greatest billing costs, with costs equal to 25.2 percent of revenue.
In contrast, inpatient stays incurred the lowest billing costs relative to the professional revenue associated with the stay. Billing costs were eight percent of revenue for a general inpatient stay and 3.1 percent for inpatient surgery.
Source: Center for American Progess
READ MORE: Paperless Medical Billing Key to Boosting Patient Collections
In addition to higher costs, insurance and medical billing also cost providers their time. The brief showed that the average processing time was 13 minutes for a primary care visit, 32 minutes for an emergency department visit, and 73 minutes for a general inpatient stay.
To bring down healthcare administrative costs for providers and payers, researchers and policymakers have been looking to countries with single payer systems.
Research shows that healthcare administrative costs are 12 percent of hospital expenditures in nations where hospitals administrators have minimal responsibilities for procuring financing and where hospital reimbursement systems are least complex. In contrast, hospital administrative costs in the US are 25.3 percent of hospital costs.
Policymakers have used the evidence to put forth single payer proposals, arguing a less complex financing system would reduce administrative burdens.
However, researchers at the Center for American Progress argued that policies targeting administrative costs alone are not enough to fix the national healthcare spending problem.
“As economists Sherry Glied and Adam Sacarny observed, ‘there are very substantial variations in administrative costs among countries with universal health insurance, which do not translate directly into variations in overall costs,’” they wrote. “Comparative evidence from US states also suggests that America’s multipayer system explains some, but by no means all, of the discrepancy between the United States and other developed nations.”
Reducing administrative costs is a key component of the national healthcare spending problem. However, prices are equally large, if not larger, issue.
A 2019 follow-up to the landmark report, “It’s the Prices, Stupid,” revealed healthcare prices are still the main driver behind excessive US healthcare spending. A separate report from Altarum also found healthcare prices hit the highest annual growth rate in six years in April 2018.
Policies aimed at reducing healthcare spending should focus on simplifying the billing and insurance process and pricing, researchers from the Center for American Progress suggested.
“A structural overhaul of how healthcare is financed and priced that includes key features of other countries’ systems—whether one payer or many—would go a long way toward eliminating excess administrative costs,” they wrote. “Simplifying the payment system should be an essential part of future health reform and would make the US system work better for taxpayers and patients alike.”
Policymakers should consider setting all-payer rates or global budgets, as well as centralizing the claims process, to bring down healthcare expenditures, they advised.
