KLAS: Quadax, SSI Group Earn Top Scores for Claims Management
Superior customer service and vendor-provider relationships earned Quadax, SSI Group, and ZirMed top marks for claims management vendors, KLAS reported.

Source: Thinkstock
- Respondents in a recent KLAS report named Quadax, SSI Group, and ZirMed as the best overall performing claims management vendors because of the high-quality customer service and support provided by the companies.
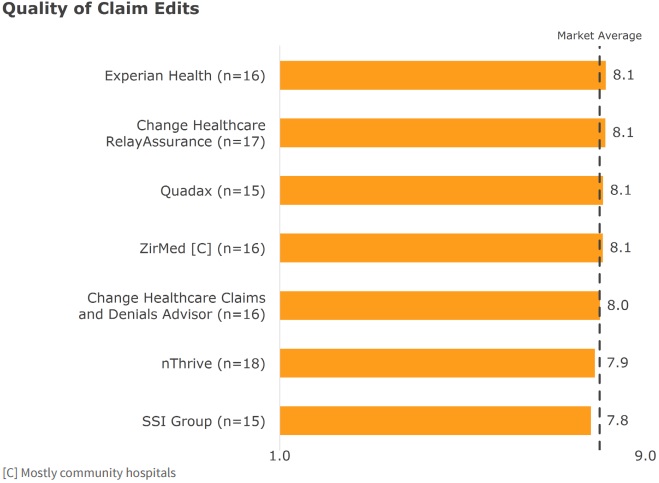
The 296 healthcare organizations interviewed by KLAS almost unanimously agreed that their claims management systems from different vendors generated high-quality claim edits, were easy to use, updated payer changes, and performed as customers expected a claims product should.
For example, claims management vendors including Experian Health, Change Healthcare, Quadax, ZirMed, nThrive, and SSI Group all ranked close to the market average for quality of claims edits.
Source: KLAS
“In this mature stage of the market, provider organizations’ revenue cycle departments generally perceive functional and accurate editing processes as a commodity,” the report stated. “What then distinguishes vendors in this high-performing market?”
Revenue cycle management leaders cited customer service and support as a top factor when identifying high-performing claims management systems and vendors. Interviewed healthcare organizations valued receiving responsive, timely, and proactive support.
READ MORE: Top Revenue Cycle Management Vendors and How to Select One
“Some of the most significant differentiators as indicated by participants in this study are found within the service delivered by the various vendors in the market,” wrote researchers. “Some vendors do much better at providing high-quality service and support, which is almost transformative in moving the experience from a vendor/customer relationship to more of a partnership.”
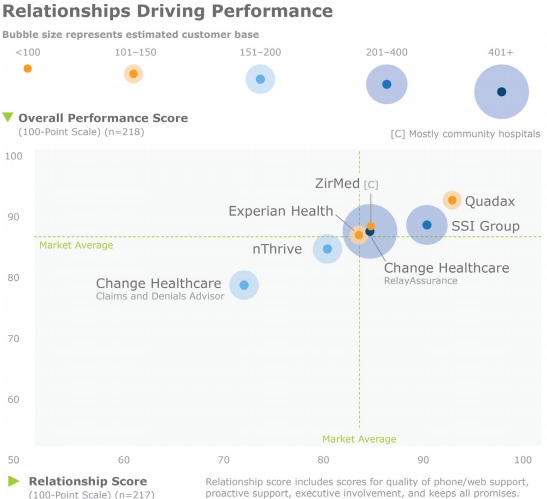
Quadax topped the chart for claims management vendors that establish partnerships with their provider organizations. The company started in the MidWest, but has gradually expanded to provide organizations in the South and East.
Source: KLAS
Despite the vendor’s limited geographical reach, Quadax emerged as a customer service performance leader. Respondents ranked the company’s quality of phone and web support 8.5 out of 9 points. The vendor’s executive involvement and proactive service also earned scores of 8.1 and 8.4, respectively.
Quadax’s customer service and relationship development contributed to the company earning the top spot for overall claims management vendor performance.
SSI Group trailed Quadax, coming in as the second top performing company because of exceptional customer service and support. The Alabama-based claims management vendor’s relationships with customers were ranked slightly behind Quadax.
READ MORE: Key Ways to Improve Claims Management and Reimbursement in the Healthcare Revenue Cycle
Respondents also gave SSI Group’s quality of phone and web support 8.3 points, proactive service 7.9 points, and executive involvement 7.6 points.
Rounding out the top three claims management vendors list was ZirMed, which was primarily used in community hospitals. The company headquartered in Kentucky was closer to the market average for relationship development.
However, ZirMed outranked SSI Group on other customer service and support factors. Respondents gave the vendor 8.3 points for quality of phone and web support and 8.1 points for proactive services.
ZirMed notably earned the least amount of points for executive involvement among all the vendors studied. But researchers noted that the score is based on limited data.
Other top-ranked claims management vendors according to customer service and relationship development included Change Healthcare’s RelayAssurance, Experience Health, and nThrive.
READ MORE: Top 4 Claims Denial Management Challenges Impacting Revenue
KLAS researchers noted that recent company mergers and acquisitions involving the top claims management vendors created customer service and relationship development issues for healthcare organizations.
Both nThrive and Change Healthcare underwent a merger and acquisition project in the last year. Customer service from some healthcare organizations suffered after the transactions were completed.
“Currently, customer feedback regarding nThrive’s support and the support received by Change Healthcare’s Claims and Denials Advisor customers is a mixed bag between those who feel the vendors have continued to provide responsive, proactive, and effective support and those who have seen the quality of their support drop,” the report stated.
Lack of continuity was a major issue after the MedAssets and Precyse merger to create nThrive. Some customers stated that customer service significantly dropped, with response times slowing.
Greater high-level turnover contributed to customer services issues after Emdeon rebranded to Change Healthcare and merged with McKesson Technology Solutions. The merger involved McKesson’s RelayHealth systems, including the RelayAssurance claims management platform.
Acute care organizations primarily used the RelayAssurance system under McKesson, while Change Healthcare’s Claims and Denials Advisor was a leader in the ambulatory space. Organizations that used the Change Healthcare solution particularly reported disruptions in service and unresolved issues, with one respondent citing high turnover as the reason.
Despite customer service issues at nThrive and Change Healthcare, some respondents still experienced high-quality customer service post-merger and acquisition.
The report’s findings of customer service issues after a merger and acquisition could spell trouble for top-ranking ZirMed. The healthcare revenue cycle management company recently announced that it will merge with Navicure. The $750 million deal is expected to close by the end of 2017.
KLAS researchers stated that a merger and acquisition should be an opportunity for claims management vendors to “take steps to make sure all organizations across their customer base are receiving the same support.”
