MSSP Accountable Care Organizations Saved Medicare Nearly $2.7B
Accountable care organizations (ACOs) in Medicare’s largest program saved about $1 billion more from 2013 to 2016 than CMS estimated, an analysis shows.

Source: Thinkstock
- Accountable care organizations (ACOs) in the Medicare Shared Savings Program (MSSP) saved more than previously thought, according to a new analysis.
The updated analysis of MSSP ACO savings from the National Association of ACOs (NACCOS) showed that organizations in the largest ACO program saved Medicare nearly $2.7 billion to date, approximately $1 billion more than the savings estimated by CMS.
“These results are the latest data point in a growing body of evidence unequivocally proving ACOs’ value,” Clif Gaus, ScD, President and CEO of the National Association of ACOs (NAACOS) stated in a press release. “ACOs are saving American taxpayers hundreds of millions of dollars at a time when it’s most needed.”
The independent evaluation conducted by the analytic firm Dobson | DaVanzo & Associates used program data from the 2013 performance year, which was the first full year of the program, through the 2016 performance year.
The data uncovered that MSSP ACOs saved about $859 million in 2016. Combining 2016 savings with the results from the previous analysis on 2013 through 2015 savings, researchers calculated not only greater overall savings, but also greater net savings.
READ MORE: For Ongoing ACO Shared Savings, Look Outside Inpatient, Primary Care
MSSP ACOs generated net savings of approximately $665.8 million from 2013 to 2016 after accounting for incentive payments made by and to the program.
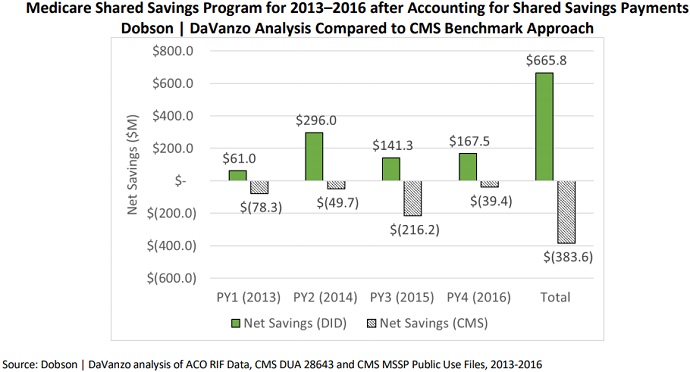
Source: National Association of ACOs (NACCOS)
Once again, the findings were significantly different from the CMS savings calculation, the analytic firm stated. CMS estimates that MSSP ACOs actually lost Medicare money, netting a financial loss of $384 million.
Researchers explained that their analysis uncovered significantly more savings from MSSP ACOs to date because of how CMS estimated savings from the program. CMS calculates MSSP ACO savings using performance data based on benchmarks, or an ACO’s annual, predetermined spending target.
Using spending targets underestimates ACO performance on savings, the analytic firm elaborated.
Other industry experts have agreed with the statement that using financial benchmarks to estimate ACO savings is not the most accurate methodology.
READ MORE: Time Helps Accountable Care Organizations Realize Savings in MSSP
“It is important to avoid using the Centers for Medicare and Medicaid Services’ (CMS’s) benchmarks to evaluate ACO savings because benchmarks are constructed with policy goals in mind,” wrote experts from Harvard Medical School in a 2017 Health Affairs blog post. “Benchmarks are not designed to reflect the counterfactual scenario in which the providers were not under the ACO contract.”
The Harvard Medical School professors and research assistant explained that a counterfactual scenario in which CMS analyzes healthcare costs if ACOs did not exist would more accurately estimate the real savings from the organizations.
Dobson | DaVanzo & Associates performed a similar analysis to determine MSSP ACO savings to date. The firm compared ACO spending to similar non-ACO providers to find what spending would be like if the ACOs did not exist.
As a result, the firm found additional MSSP ACO savings compared to CMS estimates, which relied on benchmark comparisons.
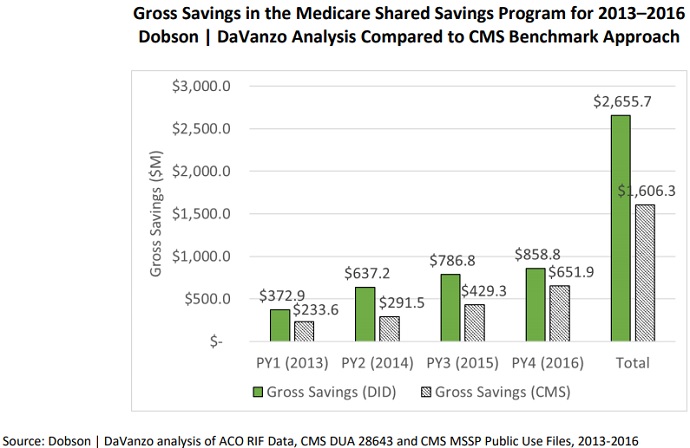
Source: National Association of ACOs (NACCOS)
“Given the natural lag time in collecting and analyzing data and the well-established trend that ACOs need a few years to start demonstrating results, we are only seeing the beginning of the nation’s return on investment in accountable care,” Gaus said. “This data doesn’t even mention the quality benefits ACOs have generated, which have also been substantial.”
READ MORE: Key Issues Impacting Two-Sided Risk Accountable Care Organizations
ACOs aim to improve fragmented, high-cost care by bringing together local physicians, hospitals, and other providers to take responsibility for the care quality and costs of a population’s healthcare. The ACO model incentivizes providers to work together for care quality and cost improvements by giving them the opportunity to earn back a portion of the savings by meeting predetermined spending and care quality goals.
The MSSP is the largest ACO program to date. Launching in 2012, the program has grown to 561 organizations covering 10.5 billion Medicare fee-for-service beneficiaries.
The MSSP may be popular among providers. But CMS has identified several challenges with the program, including a lack of two-sided financial risk adoption. Eight-two percent of ACOs are still in a shared savings-only track, which means the organizations do not have to repay CMS for potential financial losses.
“After six years of experience, the time has come to put real ‘accountability’ in Accountable Care Organizations. Medicare cannot afford to support programs with weak incentives that do not deliver value,” stated CMS Administrator Seema Verma in August 2018. “ACOs can be an important component of a system that increases the quality of care while decreasing costs; however, most Medicare ACOs do not currently face any financial consequences when costs go up, and this has to change.”
To improve the MSSP, CMS recently proposed to transform the program into the “Pathways to Success” initiative. Pathways to Success would have two versus four tracks. The Basic track would be the shared savings-only, beginners’ path and the Enhanced track would be the two-sided financial risk path.
Notable differences between the MSSP and Pathways to Success include a faster transition to the two-sided financial risk track, increased benefits for ACOs in two-sided risk arrangements, and longer agreement periods.
CMS projects the proposed MSSP transformation to save Medicare $2.2 billion over the next decade.
Industry groups have criticized the Pathways to Success proposal. NAACOS said the “administration’s proposed changes to the ACO program will halt transformation to a higher quality, more affordable, patient-centered healthcare industry.”
About 60 percent of ACO respondents in a recent NAACOS survey stated that they opposed the proposed changes, and over one-third (36 percent) would leave the MSSP if CMS finalizes the proposed changes.
On the other hand, supporters contend the proposed changes are a step in the right direction for ACOs.
“While we never want providers to take on risk before they are ready, we support the policy direction that CMS is taking because it continues to move the industry in the direction of accepting downside risk,” said Jeffrey Hulburt, President and CEO of Beth Israel Deaconess Care Organization (BIDCO), an ACO in Massachusetts. “We look forward to having a meaningful conversation with CMS, as we are positive we can provide additional feedback on how to balance the need to take on more risk while meeting providers’ needs.”
CMS anticipates a summer 2019 start date for Pathways to Success. However, the federal agency has yet to finalize program details.
