Physician-Sponsored Accountable Care Organizations Succeed
The study results illustrate that physician-sponsored accountable care organizations tended to perform at higher levels than hospital-sponsored networks.

- The Centers for Medicare & Medicaid Services (CMS) is constantly attempting to reform and modify current programs in order to achieve the Triple Aim of Healthcare – reduced medical costs, better health outcomes, and improved patient satisfaction. The provisions surrounding accountable care organizations is no different, as CMS has developed a Next Generation Accountable Care Organization.

Last week, the CMS Innovation Center announced the Next Generation ACO Model’s second round of applications. The second performance year for these specific accountable care organizations will occur on January 1, 2017.
The request for application and general information related to the Next Generation ACO Model can be found here. The CMS Innovation Center, which exists due to provisions within the Affordable Care Act, has created this new payment and care delivery system in an effort to improve upon the Medicare Shared Savings Program and older versions of accountable care organizations.
“The Next Generation ACO Model is an initiative for ACOs that are experienced in coordinating care for populations of patients,” the CMS website stated. “It will allow these provider groups to assume higher levels of financial risk and reward than are available under the current Pioneer Model and Shared Savings Program (MSSP). The goal of the Model is to test whether strong financial incentives for ACOs, coupled with tools to support better patient engagement and care management, can improve health outcomes and lower expenditures for Original Medicare fee-for-service (FFS) beneficiaries.”
“Included in the Next Generation ACO Model are strong patient protections to ensure that patients have access to and receive high-quality care. Like other Medicare ACO initiatives, this Model will be evaluated on its ability to deliver better care for individuals, better health for populations, and lower growth in expenditures.”
“This is in accordance with the Department of Health and Human Services’ ‘Better, Smarter, Healthier’ approach to improving our nation’s health care and setting clear, measurable goals and a timeline to move the Medicare program -- and the health care system at large -- toward paying providers based on the quality rather than the quantity of care they provide to patients. In addition, CMS will publicly report the performance of the Next Generation Pioneer ACOs on quality metrics, including patient experience ratings, on its website.”
The new model of healthcare delivery uses many of the building blocks and lessons learned from the Medicare Shared Savings Program and the Pioneer ACO Model. These new accountable care organizations will encompass achievable financial targets and offer more opportunity for multiple providers to better coordinate care. Most importantly, the Next Generation ACO Model aims to meet high quality measures in healthcare delivery.
The biggest difference between the Next Generation ACO Model and prior accountable care organizations working with CMS is that the newest healthcare delivery system will take on more financial and clinical risk. Greater performance risk also offers these ACOs a chance to share in greater savings.
The Next Generation ACOs have greater flexibility in their payment opportunities as well as more foreseen benchmarks that target providing higher quality services and better patient care. At this point in time, 21 Next Generation Accountable Care Organizations exist around the nation and serve patients from one coast to the other.
Any healthcare networks and organizations looking to join the Next Generation ACO Model must first submit a letter of intent, CMS reports. Open Door Forums (ODFs) will also be held by the CMS Innovation Center to clarify how to apply to be part of the new ACO model. The next Open Door Forum is to be held on Tuesday, March 22.
“Whether in the end, the program will have net savings; I think remains to be seen. I’m optimistic that it will. As Pioneer has done, it’s shown that they can find savings and improve quality. These are the most experienced organizations in our country when it comes to managing cost and quality,” Clif Gaus, the President and CEO of the National Association of ACOs, told HealthPayerIntelligence.com.
“I’m somewhat optimistic that it will be successful, but it’s such a small part of the accountable care movement, that it, in my view, isn’t where all the focus should be. The focus should be on the 400+ organizations that are in the Medicare Shared Savings Program, as only 22 are full-risk. The majority of the ACOs – 95 percent of ACOs in country – share savings with CMS and use their own money to do that.”
When it comes to determining the future success of an accountable care organization, one study outlined whether physician group or hospital sponsored ACOs are able to bring the highest level of value for the healthcare industry.
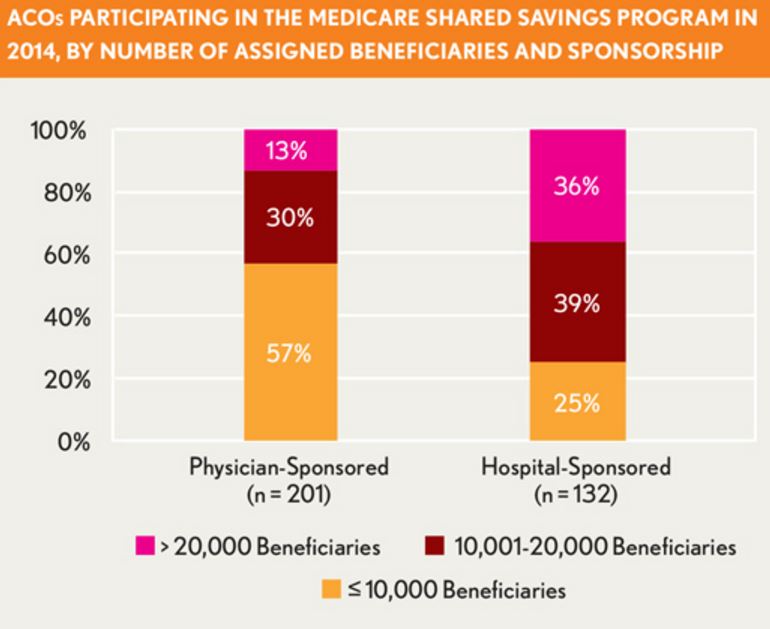
The researchers looked at the results of accountable care among physician and hospital sponsored organizations within the Medicare Shared Savings Program. Currently, 434 ACOs exist in the Medicare Shared Savings Program and both sponsorship groups run in much the same way, which makes it easier to compare and contrast their outcomes.
The results show that in 2014, only 28 percent of MSSP ACOs generated cost savings more than their minimum savings rate and were able to share in the monetary reductions. The study results illustrate that physician-sponsored accountable care organizations tended to perform at higher levels than hospital-sponsored networks.
In 2014, 31 percent of physician-sponsored ACOs met their minimum savings rate while only 22 percent of hospital-sponsored networks met this same rate. Additionally, physician-sponsored accountable care organizations were more likely to advance in quality performance when compared to hospital-sponsored ACOs.
The research study also found that cost savings were more likely to be achieved two years in a row among physician-sponsored ACOs. It is believed that the motivation to reduce healthcare spending is more straightforward and less convoluted among physician-sponsored ACO networks when compared to those sponsored by hospitals.
The study advises ACOs to find “action-oriented leadership” as well as work toward keeping emergency department visits low in order to succeed and gain cost savings. Those looking to apply for a Next Generation ACO Model through the CMS Innovation Center may want to consider being sponsored by physician groups instead of hospital-based systems.
Image Credits: Healthcare Financial Management Association