Surveys Reveal MACRA Implementation, QPP Knowledge Lacking
Only about half of providers feel knowledgeable about MACRA implementation and the QPP, while executives thought they understood more than they did.

Source: Thinkstock
- Two recent surveys indicated that healthcare provider and executive knowledge of and readiness for MACRA implementation and the Quality Payment Program are lacking despite the value-based reimbursement program launching in January 2017.
A new Nuance Communications survey revealed that 61 percent of hospital finance executives are confident that they understand MACRA implementation and Quality Payment Program requirements.
Another 56 percent of respondents reported that they were ready to meet Quality Payment Program reporting requirements.
However, over three-quarters of executives who said they were somewhat or very confident in their Quality Payment Program understanding did not correctly identify the greatest Merit-Based Payment System (MIPS) penalty eligible clinicians could receive based on 2017 performance. The penalty maximum is 4 percent.
Sixty percent of those reportedly knowledgeable about the Quality Payment Program also underestimated or did not know the financial impact of the value-based reimbursement program.
In addition, hospital finance executives lacked understanding about Quality Payment Program reporting requirements. Only 35 percent of participants who said they were confident with their Quality Payment Program understanding correctly stated that the program requires 90 days of quality data to be submitted.
One-half of executives either underestimated or did not know the number of days required for data submission.
“Without proper clinical documentation, no organization will do well with QPP [Quality Payment Program],” stated Anthony Oliva, MD, Nuance Chief Medical Officer. “While the changes are daunting, it is crucial for hospitals and clinicians to take proactive steps to prepare, plan and participate. Doing so will help organizations retain what they earn in the short term, but will also set them up to avoid severe penalties in the long run.”
A recent American Medical Association (AMA) and KPMG survey uncovered similar MACRA implementation and Quality Payment Program challenges. The survey of 1,000 practicing providers who are involved in practice decision-making for MACRA implementation showed that providers are split on how well they understand the Quality Payment Program.
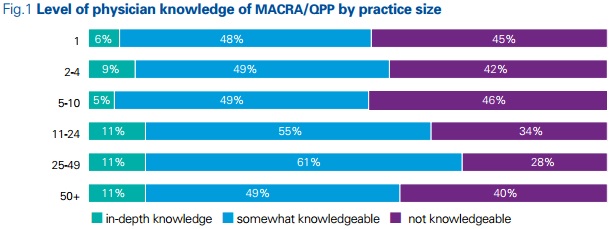
About one-half (51 percent) of respondents said they were somewhat knowledgeable of MACRA and the Quality Payment Program. Another 41 percent stated that they had heard of the program, but would not identify themselves as knowledgeable.
Only 8 percent of providers reported that they were deeply knowledgeable about the Quality Payment Program.
Providers in large practices of at least 10 physicians tended to report higher levels of MACRA implementation understanding with 11 percent saying they are deeply knowledgeable versus those in smaller practices (6 percent of solo providers, 9 percent of those in practices of two to four physicians, and 5 percent for those in practices of five to ten physicians).
Source: American Medical Association, KPMG
Specialists and primary care were equally as likely to say they were deeply knowledgeable with 9 percent and 7 percent, respectively. About one-half of each provider type also stated they were somewhat knowledgeable.
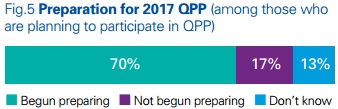
Despite a lack of overwhelming Quality Payment Program and MACRA implementation understanding, about 70 percent of providers said their practices have started to prepare for the Quality Payment Program in 2017.
Source: American Medical Association, KPMG
Most respondents (65 percent) stated that they are somewhat ready for meeting Quality Payment Program reporting requirements in 2017. Just 23 percent of these providers felt well prepared.
Only 17 percent stated that their practice has not prepared and 13 percent are not sure.
As part of their Quality Payment Program preparation, most practices have decided on their Quality Payment Program track. Approximately 56 percent of providers plan to participate in MIPS in 2017 and roughly two in ten anticipate joining an Advanced Alternative Payment Model (APM).
Out of the providers expecting to participate in MIPS, about three in ten plan to take advantage of the Quality Payment Program transition period and just report one measure in 2017. About 76 percent of these providers expect to submit data on a quality measure versus Advancing Care Information and Improvement Activities measures.
The other top 2017 MIPS reporting paths providers planned to use included:
• About 25 percent expect to report partially, with more than one measure submitted
• Approximately 30 percent anticipate full MIPS reporting
• 2 percent plan to report as a MIPS APM
• 12 percent said they do not know what level of MIPS reporting their organization plans to do
While most providers have made a plan for MACRA implementation, challenges remain. About 90 percent of providers anticipating reporting to MIPS stated that MIPS requirements are very burdensome (53 percent) or slightly burdensome (37 percent).
In addition to reporting burdens, respondents also identified the following MACRA implementation obstacles:
• Time required to accurately gather and report performance data with 66 percent of respondents
• Understanding reporting requirements with 58 percent
• Understanding overall MIPS scoring processes with 57 percent
• Cost needed to accurately gather and report performance data with 53 percent
• Organizational infrastructure required to report performance with 49 percent
“Aligning physician incentives with quality and other performance targets will lead to greater rewards for physicians and better healthcare for patients,” said S. Lawrence Kocot, KPMG National Leader of the Center for Healthcare Regulatory Insight. “While progress has been made in preparing physicians for the move from volume in the fee for service payment model to value in alternative payment models, it is important that we do even more to assist physicians with the transition.”
