Understanding 2017 MIPS Quality, Cost Performance Categories
At HIMSS17, a CMS director elaborated on the MIPS quality and cost performance categories in 2017 and advised clinicians on how to report for maximum reimbursements.

Source: Thinkstock
- CMS leaders at HIMSS17 were not shy with telling session attendees that they are currently in the first Quality Payment Program performance year. To help providers better understand the program, which launched on Jan. 1, the federal agency’s staff elaborated on how providers can report on certain Merit-Based Incentive Payment System (MIPS) categories.
While the Quality Payment Program offers two value-based reimbursement tracks, CMS anticipates about 592,000 to 642,000 eligible clinicians to participate in MIPS during the 2017 transition year.
With most eligible clinicians under the MIPS track this year, Reena Duseja, MD, CMS Director for the Division of Quality Measurement, provided HIMSS17 attendees with more information on the MIPS quality and cost performance categories.
She started by explaining that MIPS reporting requirements in 2017 are more flexible because the final MACRA implementation rule codified flexible attestation options during the first performance year. But eligible clinicians must submit some data to avoid a negative Medicare payment adjustment in 2019.
To prevent a financial penalty, eligible clinicians must submit data on a MIPS quality measure, improvement activity, or all the required advancing care information measures. Submitted data must cover at least a 90-day period, but could include a full year period.
READ MORE: What We Know About Value-Based Care Under MACRA, MIPS, APMs
“We want to stress with these performance categories is that we are trying to provide clinicians with flexibility,” Duseja said. “We want you to be able to choose activities and measures that are the most meaningful to your practice.”
The MIPS cost category will also not be counted for Medicare payment adjustments during the transition year, Duseja reminded attendees. However, eligible clinicians will be assessed on their cost management performance starting in 2018.
Even though quality and cost measures may not be on the minds of all eligible clinicians this year, the CMS director went over the MIPS quality and cost performance categories to help participants better understand the measures and how to maximum Medicare reimbursement under the program in 2017.
MIPS quality performance category
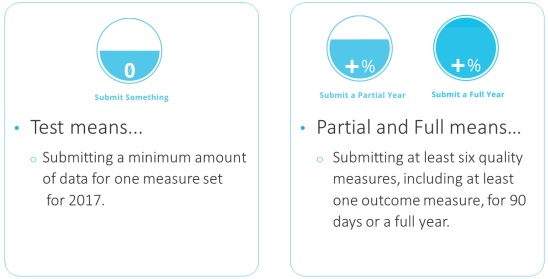
In 2017, eligible clinicians have the option of submitting one to six MIPS quality performance measures, Duseja explained. For clinicians electing to just test the Quality Payment Program, submitting data on one quality measure for 90 days will prevent them from seeing a downward Medicare payment adjustment in 2019.
Clinicians can also potentially earn higher positive Medicare payment adjustments in 2019 by submitting data on more measures. By providing data on at least three quality measures, clinicians will follow a partial MIPS participation plan and qualify for a higher adjustment.
READ MORE: CMS Timelines for Stage 3 Meaningful Use, MACRA Implementation
Even greater Medicare payment adjustments will be available to clinicians who fully participate by submitting data on at least six quality measures.
Source: CMS
MIPS clinicians have 271 quality measures to choose from in 2017, Duseja added. For maximum Medicare payment adjustments, clinicians must submit data on the six measures with one being an outcome or high-priority measure.
If an outcome measure is not appropriate for a clinician, he can choose a high-priority measure, she noted. CMS defines a high-priority measure as an outcome, appropriate use, patient experience, patient safety, efficiency, or care coordination measure.
In addition, CMS included specialty-specific measure sets for clinicians operating in a more specialized practice.
Clinicians reporting as group that has 16 or more eligible clinicians will also automatically be evaluated on a readmission measure as long as they have 200 or more cases. There is no requirement to submit data on this measure.
READ MORE: Preparing the Healthcare Revenue Cycle for Value-Based Care
Duseja noted that the MIPS quality measures are similar to the Physician Quality Reporting System (PQRS), but MIPS reduced the reporting burden on clinicians.
“The six measures that clinicians are going to be reporting on under MIPS is actually a decrease from what is required under the PQRS,” she stated. “Under PQRS, clinicians were required to report on nine measures that cover three national quality strategy domains.”
“Within MIPS, there’s no requirement that clinicians would have to choose measures that cover a certain number of domains,” she continued. “Rather clinicians are encouraged to choose measures in as many domains as possible.”
For clinicians fully participating in 2017, the quality component of MIPS will represent 60 percent of the total MIPS performance score. Each quality measure is worth up to 10 points based on performance benchmarks.
Failing to submit data on a quality measure will result in zero points, whereas submitting sufficient data will automatically earn a clinician 3 points in 2017.
Clinicians can earn more than 3 points if the measure can be “reliably scored against a benchmark.” According to Duseja, a reliable score means that there is sufficient case volume (20 or more cases for most measures), data is complete (at least 50 percent of possible data submitted), and a benchmark exists for the measure.
“The key here is that if you are really looking to receive more than the 3 points, you want to be participating longer so you’re meeting the case volume criteria for that measure to be within that benchmark,” she said.
CMS determines each measure’s benchmark based on the reporting mechanism. Therefore, the following will have separate benchmarks:
• EHRs
• Qualified Clinical Data Registry and other registries
• CMS Web Interface
• Administrative claims measures
• Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey for MIPS
If a benchmark is not available for a certain measure, then clinicians will automatically receive 3 points for submitting data on that measure.
Clinicians can also earn bonus quality performance points in 2017. For one extra point, clinicians can submit an additional high-priority measure and two bonus points will be awarded for submitting data on additional outcome and patient experience measures.
Two bonus points will also go to clinicians who use certified EHR technology to submit data. Another bonus point is also available if data is submitted “electronically end-to-end.”
Once data is sent to CMS, the federal agency will calculate a total quality score. The score will be determined using the following equation:
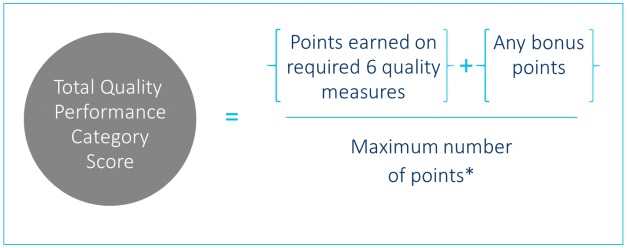
Source: CMS
The maximum points available in the quality category is 60 points, unless a group of 16 or more clinicians qualifies for the readmission measure, in which case the maximum points will be 70 points.
Duseja also pointed out that CMS developed different maximum points and measure requirements for groups reporting through the CMS Web Interface.
MIPS cost performance category
The MIPS cost performance category will not be weighed in 2017 final performance scores, Duseja explained.
“The rationale behind this was to really have clinicians understand what cost measurement is. It’s a relatively new concept for providers,” she said. “We also eliminated the cost category’s weight in 2017 to really get as much feedback as we can get from the community and stakeholders as we’re developing the measures.”
Despite having no impact on 2019 MIPS payment adjustments, CMS will still provide feedback to providers on how they performed on cost in 2017. The federal agency will use Medicare claims data to assess eligible clinicians on measures already used in the Physician Value-Based Modifier program and those used in the Quality and Resource Use Report.
The cost measures used in 2017 will be Medicare spending per beneficiary, total spending per capita, and ten episode groups. Clinicians will not need to submit data on these measures.
While CMS has not finalized cost measures for MIPS, Duseja elaborated on how the federal agency intends to define the measures. At the most basic level, the cost evaluations will be based on “Medicare payments for items and services furnished to a beneficiary during an episode of care.”
Each care episode will be defined as the “items and services through claims that are furnished to address a condition within a specified timeframe.”
More specifically, CMS will develop cost measures using the following five components:
• Define an episode group
• Determine costs for an episode group
• Attribute the episode group to one or more responsible clinicians
• Risk adjust an episode group to compare like beneficiaries, such as case mix
• Align an episode group’s costs with quality indicators
MIPS cost measures will also be divided into three episode groups. The divisions are chronic condition, acute inpatient medical condition, and procedural episode groups.
“Our goal with these cost measures is to align as much as possible with our quality measures,” Duseja stated. “The goal behind having this category is for all of us to think smartly about how do we improve patient outcomes and how do we spend smarter in terms of how we are taking care of our patients.”
She added that CMS is seeking more stakeholder feedback for MIPS cost measure development. All stakeholders can comment on the federal agency’s approach to cost measure development on the CMS website until April 24, 2017.
While cost performance may not make Quality Payment Program top priority lists in 2017, eligible clinicians may consider using the transition year to learn more about the MIPS category before it launches in the 2018 performance year.
