Value-Based Payment Opens Doors for Better Opioid Use Disorder Care
Shifting from fee-for-service to value-based payment will open the door and keep it unlocked for substance and opioid use disorder patients struggling to access coordinated care.

Source: Getty Images
- Nearly 64,000 Americans died from a drug overdose in 2016 alone, with opioid overdoses representing over 42,000 of those deaths, more than any previous year on record. It was that figure – as well as many other troubling statistics – that prompted the Trump administration in October 2017 to declare the opioid crisis as a public health emergency.
America is no stranger to drug addiction, but the addiction landscape is a lot different compared to decades ago. Drug overdoses accounted for the deaths of nearly 400,000 Americans from 1999 to 2017, making it the leading cause of injury-related deaths in the US, CDC reported.
However, the number of overdose deaths in 2017 involving opioids, including prescription opioids, illegal opioids like heroin, and illicitly manufactured fentanyl, was six times higher than in 1999, the department found.
The most current administration has dedicated over $1 billion to address the opioid crisis and drug addiction in the US. It has also developed a strategy to combat opioid abuse, misuse, and overdose, with improving access to prevention, treatment, and recovery services being the main pillar.
The grants, awards, and other resources are helping healthcare stakeholders bolster opioid and substance use disorder (SUD) treatment. But the healthcare industry may already hold the key to more long-lasting, sustainable access to care improvements.
“To successfully implement the cascade treatment of care framework in a sustainable manner, incentives are necessary to encourage providers to use quality measures, report on their performance, and develop quality improvement plans. Value-based payment models can potentially facilitate the upscale implementation of the cascade treatment of care framework,” researchers from Columbia University and the New York State Psychiatric Institute wrote in Health Affairs in 2018.
Value-based payment models tie provider reimbursement to clinical and/or financial outcomes to incent providers to deliver higher quality care at lower costs and coordinate care across the continuum. The models have been largely successful in treating patients with chronic conditions or who experience well-defined episodes of care, such as a joint replacement.
The models also have the potential to significantly improve SUD, and specifically opioid use disorder (OUD).
“If you had this coordinated care model, you'd be driving towards some outcomes,” said Shawn Ryan, MD, MBA, FASAM, board-certified emergency and addiction physician and chair of legislative advocacy at American Society of Addiction Medicine (ASAM).
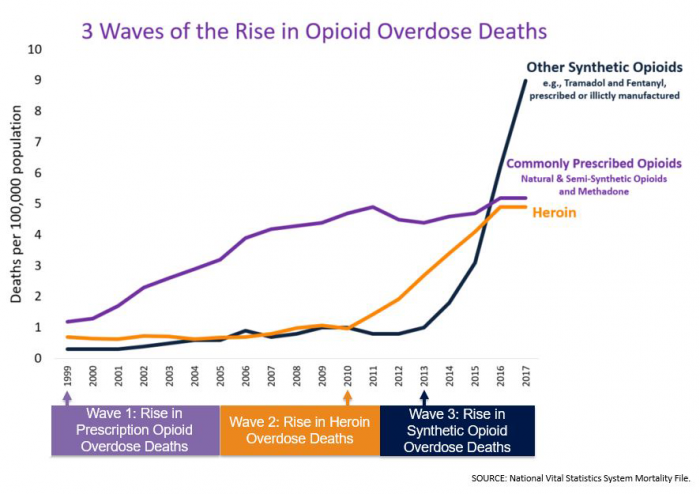
Source: Centers for Disease Control and Prevention
The failures of fee-for-service
Value-based payment models promise to improve patient outcomes and reduce costs by transforming the reimbursement system to pay for value of care, not volume of services. But the industry is still very much entrenched in fee-for-service.
Just over one-third of healthcare payments were tied to a bundled payment, shared savings contract, population-based arrangement, or other alternative payment model in 2018, according to the latest numbers from the Health Care Payment Learning & Action Network.
Straight fee-for-service or value-based models built on fee-for-service are still the main sources of revenue in healthcare. And these payment models are impeding access to care for individuals with SUD and OUD.

Greg Williams, manager of the Alliance for Addiction Payment Reform from Third Horizon Strategies
Source: Third Horizon Strategies“Substance use disorder is a very variable spectrum condition. If you line up ten people, those ten people need ten different things. Providers in a fee-for-service world don't necessarily have the flexibility to meet the needs of those patients in different ways,” explained Greg Williams, a person in long-term recovery and a manager of the Alliance for Addiction Payment Reform from Third Horizon Strategies.
And the same is likely true for patients with other chronic conditions, he continued. “Fee-for-service is a square peg in a round hole when it comes to chronic disease management. Chronic illness takes long-term management, but most of our fee-for-service services have been created in isolation and fragmentation. So, we have an infectious disease model to treat a chronic disease.”
However, SUD and OUD patients are facing worse access to care issues compared to those with traditional, “physical” conditions. Out-of-network utilization rates for behavioral health providers were higher than medical and surgical providers from 2013 to 2017, Milliman recently reported.
But even if SUD patients are accessing care, the fee-for-service model is not addressing personalized needs, if the low reimbursement rates encourage care at all, Ryan added.
“Reimbursement for the medical providers is typically in the Medicaid environment,” he explained. “The general Medicaid reimbursement for a mid-level code in a primary office – a 99213 or 4 – is completely insufficient to learn the practice. What providers generally do is not take on many Medicaid patients to offset that loss margin.”
Milliman also found similar problems in the commercial market. Average in-network rates for behavioral health office visits were lower compared to rates for medical or surgical office visits, and the disparity between the two has increased.
Even if providers are willing to see more SUD patients, the current payment system doesn’t necessarily support the services needed for individuals with this condition. Some states may have case management codes built into their Medicaid programs for services like peer or social support, but the codes promote that type of case management whether patients need it or not.

Shawn Ryan, MD, MBA, FASAM, chair of legislative advocacy at American Society of Addiction Medicine
Source: ASAM“That’s one of the failures of the fee-for-service model. It is forcing people’s hands,” Ryan stated.
Value-based payment models allow for the flexibility SUD patients and providers need to treat the disorders as chronic conditions, which require long-term, personalized treatment plans, the addiction specialists agreed. The models also encourage providers to think beyond the walls of their offices, which is crucial to effective chronic disease management.
Poor care coordination can increase chronic disease costs by $4,500 over three years, especially when the lack of coordination leads to inappropriate utilization of healthcare resources. The avoidable expenditures also have a human cost, resulting in poor clinical outcomes and frustration among patients and providers.
Providers know care coordination benefits them, their patients, and the healthcare system at large. But they can only do so much without the financial support, Ryan stated.
“People do what you pay them to do, including healthcare service providers. If you don't appropriately support the reimbursement to do the services that are indicated, evidence-based, desired, whatever version of those words you want to use, they can't or won't,” he said.
But value-based payment models can.
Developing value-based payment models for coordinated SUD, OUD care
Both ASAM and the Alliance for Addiction Payment Reform are forging a path for SUD- and OUD-specific value-based payment models.
In collaboration with the American Medical Association (AMA), ASAM released the Patient-Centered Opioid Addiction Treatment (P-COAT) model last year. Several months later, the Alliance unveiled the Addiction Recovery Medical Home Alternative Payment Model.
The organizations agreed that developing value-based payment models for SUD and OUD care takes a multi-sector partnership, as well as a bundled payment arrangement.
The P-COAT model uses a one-time payment for evaluation, diagnosis, and treatment planning for an OUD patient and the initial month of outpatient medication-assisted treatment. After that, providers receive a lower monthly payment to provide or coordinate ongoing outpatient medication, psychological, and social services.
There are also two types of bundled payments in the Addiction Recovery Medical Home Alternative Payment Model, which are supported by Remedy. The model starts with a static bundled payment, which covers the costs of high-acuity care that spans the institutional spectrum, and ends with a declining bundled payment for integrating SUD patients back into the community and promoting the continuation of treatment and recovery plans after patients successfully complete intensive outpatient services or 12 months of care.
These bundled payments lend themselves to coordinated, comprehensive SUD and OUD care, said Eric Bailly, business solutions director and head of SUD efforts at Anthem, Inc, an Alliance member organization.
“There are different ways that the payment can be approached, but the capitated bundled payments are the foundational approach that we take,” he said. “The payments enable the treatment service delivery system to deliver the different levels of care when it's most appropriate for that particular patient at the moment in time.”
So, when patients need more frequent, higher acuity services when they first start their addiction recovery journey, the bundled payments reflect that. Payment rates are higher to enable providers to deliver higher-cost care and collaborate with addiction specialists, social workers, and other providers to create a path to lower cost, more effective care down the road.
On the recovery side of addiction treatment, bundled payment rates are lower. However, the payment mechanism encourages coordinated, comprehensive care even when a patient relapses and requires services that cost more than that bundle.
“It really behooves the addiction recovery medical home to take ownership over that particular patient and to help him get the services that he needs at that moment of time to get him back on the right track,” Bailly explained. “If that means a brief stint in a residential treatment center, then that's what they'll do as part of that ecosystem.”
The bundles eliminate the incentive to maximize reimbursement at that point in the addiction recovery journey. “It's more about what we need to do to make sure that this particular patient continues to have a successful recovery journey,” he said.
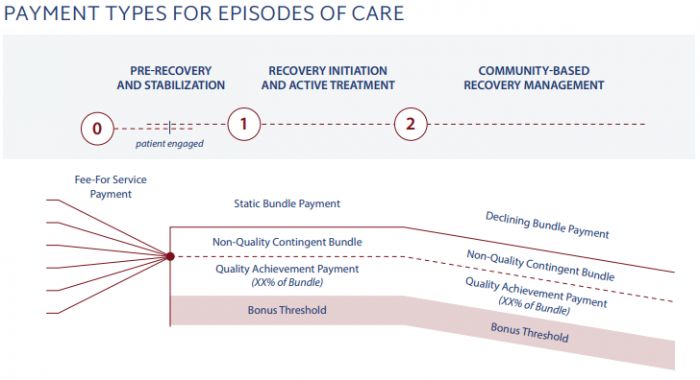
Source: Alliance for Addiction Payment Reform
Putting value-based SUD into practice
The value-based payment models have the potential to significantly reduce costs and improve patient outcomes by incenting coordinated, comprehensive SUD care. However, that is just what they are: models.
ASAM and the Alliance designed their respective SUD value-based payment models as frameworks for other stakeholders to use when developing their own contracts.
“When you build these models, there are a lot of questions. Is it over detailed? Is it under detailed? We landed in the middle because that's where you need to land generally,” Ryan explained.
For example, the P-COAT model includes bundled payments for two distinct care episodes, but the model does not specify how much those bundles should be.
“Everybody is going to set rates differently,” he said. “In every environment, you're going to have a different set of practitioners. The same is true in a smaller community versus suburban versus urban setting. We've made it flexible and, hopefully, in line with other things in the market already.”
The strategy is starting to pay off for the Addiction Recovery Medical Home Alternative Payment Model, which recently launched several demonstration projects in seven markets.
Right now, the value-based payment has attracted larger health systems and accountable care organizations (ACOs), Williams reported. These organizations generally have care coordination capabilities already in place and have more of the services needed for value-based SUD care under one roof.
Unfortunately, the value-based payment models have yet to convince many other providers to have SUD as a service line capability, according to Corbin Petro, CEO and co-founder of Eleanor Health, an outpatient addiction and mental health services provider in North Carolina modeled on value-based care delivery and payments.

Corbin Petro, CEO and co-founder of Eleanor Health
Source: Eleanor Health“Many providers, especially hospital systems, are not interested in having substance use disorder as a service line capability. And many providers, even if they're waivered to prescribe buprenorphine, aren't doing so because they don't have the wrap services,” she said.
That is where Eleanor Health steps in.
The outpatient care provider goes into a market and works with a payer to identify access gaps and create a value-based payment model to address those gaps based on the risk appetite of that payer. The provider then locates itself where patients need services, including in the hospital.
“We are pursuing some co-location models with hospital systems and providers in which we can augment the services that they're providing and have that full set of services around substance use disorder that many of these systems aren't equipped to build up themselves,” Petro explained.
Through its value-based approach, the models developed by Eleanor Health – which is also a big supporter of the bundled payment arrangement – promote coordinated SUD and OUD care.
The future of value-based SUD care
Coordinated SUD and OUD care supported by value-based payment models is still in its infancy, but the future is bright because of these first steps, the industry experts agreed.
“There are some providers out there who are really doing a wonderful job in terms of integrating physical health and behavioral health and to some extent, SUD. This takes it up a notch,” said Bailly, who is helping Anthem run pilot programs of the Addiction Recovery Medical Home Alternative Payment Model in Connecticut and Kentucky.
From his payer perspective, Bailly has noticed that providers are more willing to explore what they can do differently to support a value-based payment model for SUD now that Anthem is getting creative with payment innovation.

Eric Bailly, business solutions director and head of SUD efforts at Anthem, Inc
Source: Anthem“For instance, including peer recovery support services,” he elaborated. “That might be something that a particular ecosystem might not have in-house currently, but they may have an organization within their community that they can partner with to shore that up and fill that particular gap.”
The seeds are being planted. Providers and payers are exploring new ways to treat SUD and OUD patients in light of new value-based payment models that financially support their efforts and allow for sustainable, positive change. But time is needed for these models to bloom.
“First order of business is to get some proof of concept pilots up off the ground,” Bailly pointed out. “Once we have some data rolling in, that'll help us shift and shape how we want the model to move forward in other markets and what it is that we can bring to the table when we have these conversations with other provider entities that are interested in it. So, the analytics component will be very, very important.”
More data will also help payers and providers have a meaningful conversation at that table.
“There isn't a lot of data because there aren't many of these alternative payment models to the degree that we're talking about in the space. It’s a new frontier that we are designing, so the biggest challenge is getting aligned,” Petro stated. “Different payers have different appetites for risk and, so right now we have to be working with innovative, forward-thinking payers.”
Aligning the industry around quality measures will be a key use of the data, Petro and Williams added. Traditional SUD care models track and reward measures like negative urine drug screens and relapse rates and at this point in time, the Alliance is relying on process, rather than outcome, measures in its pilot programs.
Value-based payment models need to monitor other measures that track the value of care to the provider and patient, they agreed.
“It's really important to track a patient's sense of purpose, meaning in their life, promoter scores, longevity in treatment, access to treatment, turnaround time from when a patient calls to when they get in the door. Those are the metrics that we're valuing and trying to report on because the other metrics basically encourage a lot of these providers to fire patients,” Petro stated referring to providers who cherry-pick healthy patients to avoid financial losses or penalties.
The Alliance will evaluate and refine quality measures as the pilot programs mature, Williams reported. He also hopes to develop some of those value-adding, outcome-based quality measures based on what they learned from the pilots.
With key improvement to the models, Williams sees a way to overcome the country’s current situation, in which 130 people die from an opioid overdose per day.
“We have about a 90 percent treatment gap in this country, and it’s really important for people to wrap their minds around that. People are presenting in a lot of places where care is not offered to them and until we transform the payment model, we're not going to be able to close the addiction treatment gap,” concluded Williams.
