CMS Announces New Advanced Alternative Payment Model Options
The Oncology Care Model’s two-sided risk track will qualify as an Advanced Alternative Payment Model in 2017 and applications are re-open for two other models in 2018.

- CMS recently announced new opportunities for eligible clinicians to participate in an Advanced Alternative Payment Model (APM) under the Quality Payment Program in 2017 and 2018.

The Oncology Care Model’s two-sided financial risk track will now be available to eligible clinicians in 2017, which will qualify as an Advanced APM in the Quality Payment Program’s first performance year.
The federal agency also plans to re-open applications for practices and payers in the Comprehensive Primary Care Plus (CPC+) model and in the Next Generation Accountable Care Organization (ACO) program for the 2018 performance year. These programs are already listed as Advanced APMs.
“With these new opportunities, CMS expects that by the 2018 performance period, 25 percent of clinicians in the Quality Payment Program will earn incentive payments by being a part of these advanced models,” stated Patrick Conway, MD, CMS Deputy Administrator. “Thanks to MACRA and the Innovation Center, we’re striving to see more Medicare patients benefit from better care when they visit their doctor for a knee replacement, receive cancer treatment, or have a coordinated care team manage their complex conditions.”
Under the Quality Payment Program in 2017, eligible clinicians can earn a five percent value-based incentive payment by sufficiently participating in the following Advanced APMs:
• Comprehensive End Stage Renal Disease (ESRD) Care Model (Large Dialysis Organization Arrangement)
• Comprehensive ESRD Care Model (Non-Large Dialysis Organization Arrangement)
• CPC+
• Medicare Shared Savings Program ACOs in Track 2
• Medicare Shared Savings Program ACOs in Track 3
• Next Generation ACO program
• Oncology Care Model (two-sided financial risk arrangement)
CMS projects approximately 70,000 to 120,000 clinicians to participate in an Advanced APM during the 2017 performance year.
But the federal agency expects more than 125,000 clinicians to join an Advanced APM for the 2018 performance year. CMS plans to expand the list of Advanced APMs in 2018 by adding some Medicare Shared Savings Program ACOs in Track 1, new voluntary bundled payment models, the Comprehensive Care for Joint Replacement Model, and the Advancing Care Coordination through Episode Payment Model Track 1.
Eligible clinicians in the Comprehensive Care for Joint Replacement Model and Advancing Care Coordination through Episode Payment Model Track 1, however, will need to participate in the certified EHR technology tracks to qualify as an Advanced APM.
The final MACRA implementation rule, CMS added, lowered the risk criteria required for Advanced APM status, allowing a broader range of payment models to potentially be added to the list. For example, CMS intends to develop a Medicare Shared Savings Program Track 1 option with lower risk levels than those currently included in Medicare ACOs. The modified Track 1 option would qualify as an Advanced APM in 2018.
Additionally, CMS noted that Advanced APM participants could earn a five percent value-based incentive payment between 2019 and 2024 as well as be exempted from reporting requirements under the Merit-Based Incentive Payment System (MIPS).
After the 2026 performance year, CMS plans to modify the value-based incentive payment structure. Advanced APM clinicians who sufficiently participate would qualify for a 0.75 percent fee schedule update, while clinicians who fell below participation thresholds could earn a 0.25 percent fee schedule update and may also be subject to MIPS reporting requirements and payment adjustments.
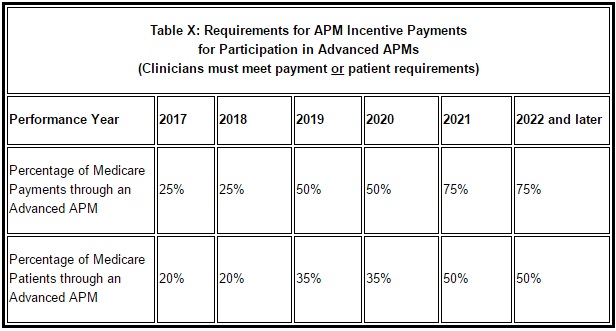
To qualify for value-based incentive payments under an Advanced APM, eligible clinicians must also receive a certain portion of their healthcare payments and see a certain portion of patients through the Advanced APM during the performance year. In 2017 and 2018, 25 percent of Medicare payments or 20 percent of Medicare patients must be associated with the Advanced APM.
The participation threshold will increase to 50 percent of Medicare payments or 35 percent of Medicare patients in 2019 and 2020. From 2021 and later, clinicians must receive 75 percent of Medicare payments or see 50 percent of Medicare patients through the model.
However, CMS added that participation thresholds will apply to all healthcare payments and patients starting in the 2019 performance year.
While CMS recently announced new Advanced APM opportunities, the federal agency still plans to release a finalized list of approved models for the first performance period by Jan. 1, 2017. It also anticipates publishing a final 2018 list before the start of the second performance year.
CMS plans to work with the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to review and evaluate potential models. The committee was established by the final MACRA implementation rule and is designed to develop provider-focused models that reduce cost and/or improve care quality.
“Now, thanks to the bipartisan MACRA, clinicians have more opportunities and motivation to join these evidence-based approaches, which aim to improve care quality while creating cost savings,” said CMS Acting Administrator Andy Slavitt.
The recent CMS announcement may seem a step in the right direction for some healthcare industry groups, like the American Hospital Association (AHA), that were disappointed by the narrow list of Advanced APMs in the final rule.
“While we are disappointed that CMS continues to narrowly define Advanced Alternative Payment Models, which means that less than ten percent of clinicians will be rewarded for their care transformation efforts, we are encouraged that CMS is exploring a new option that would expand the available advanced APMs that qualify for incentives,” Tom Nickels, AHA Executive Vice President, stated in a press release last week.
Image Credit: CMS
Dig Deeper:
• Impact of Quality Payment Program on Medicare Reimbursement
• What We Know About Value-Based Care Under MACRA, MIPS, APMs
