What Is Value-Based Care, What It Means for Providers?
Value-based care has emerged as an alternative and potential replacement for fee-for-service reimbursement based on quality rather than quantity.

Source: Getty Images
- Value-based care is a form of reimbursement that ties payments for care delivery to the quality of care provided and rewards providers for both efficiency and effectiveness. This form of reimbursement has emerged as an alternative and potential replacement for fee-for-service reimbursement, which pays providers retrospectively for services delivered based on bill charges or annual fee schedules.
In order to transform how healthcare providers are reimbursed for services rendered, the Centers for Medicare & Medicaid Services (CMS) has itself introduced an array of value-based care models, such as the Medicare Shared Savings Program, Next Generation ACO Model, and Pioneer Accountable Care Organization (ACO) Model. Private payers have, in turn, adopted similar models of accountable, value-based care.
While the traditional fee-for-service reimbursement model promoted the quantity of services, federal officials have proposed several reimbursement programs that reward healthcare providers for the quality of care that they give to patients. Value-based care seeks to advance the triple aim of providing better care for individuals, improving population health management strategies, and reducing healthcare costs.
In more basic terms, value-based care models center on patient outcomes and how well healthcare providers can improve quality of care based on specific measures, such as reducing hospital readmissions, using certified health IT, and improving preventative care.
The Department of Health & Human Services (HHS) set a goal of converting 30 percent of fee-for-service Medicare payments to value-based payment models by the end of 2016. The agency also expected 50 percent of traditional payments to make the transition by 2018.
Yet, data shows that only 38.2 percent of healthcare dollars flowed through some type of value-based payment model as of 2019.
As the healthcare industry transitions to this new way of delivering care, many healthcare providers are left wondering how value-based care differs from the traditional model, what programs are available, and how successful it has been?
The following sections will examine the basics of value-based care and help readers understand how the model works.
HOW IS VALUE-BASED CARE DIFFERENT FROM FEE-FOR-SERVICE MODELS?
In the traditional fee-for-service reimbursement model, healthcare providers were paid for the number of services they performed. This has incentivized many providers to order more tests and procedures and manage more patients to get paid more.
The costs were determined by what commercial payers would pay in the private market and a percentage of what Medicare would have paid for similar services. Rates for services were also unbundled, meaning each service was paid for separately.
“The goal is straightforward but ambitious: Replace the nation’s reliance on fragmented, fee-for-service care with comprehensive, coordinated care using payment models that hold organizations accountable for cost control and quality gains.”
Under fee-for-service models, cost variations for procedures and tests increased, and the healthcare industry was spending more to treat patients even though patient outcomes were not necessarily improving. The model also challenged provider workflows because physicians saw more patients, and each claim had to be processed in a fragmented network.
The federal government designed value-based care programs to drive down healthcare costs and improve patient outcomes. These reimbursement and care models hinge on advancing quality of care while increasing patient access and accounting for price at the point of care.
“The opportunity exists to transform how healthcare is delivered,” explained a State Health Care Cost Containment Committee report. “The goal is straightforward but ambitious: Replace the nation’s reliance on fragmented, fee-for-service care with comprehensive, coordinated care using payment models that hold organizations accountable for cost control and quality gains.”
Value-based reimbursements are calculated by using numerous quality measures and determining the overall health of populations. Unlike the traditional model, value-based care is driven by data because providers must report to payers on specific metrics and demonstrate improvement. Providers may have to track and report on hospital readmissions, adverse events, population health, patient engagement, and more.
Under the new models, providers are incentivized to use evidence-based medicine, engage patients, upgrade health IT, and use data analytics to get paid for their services. When patients receive more coordinated, appropriate, and effective care, providers are rewarded.
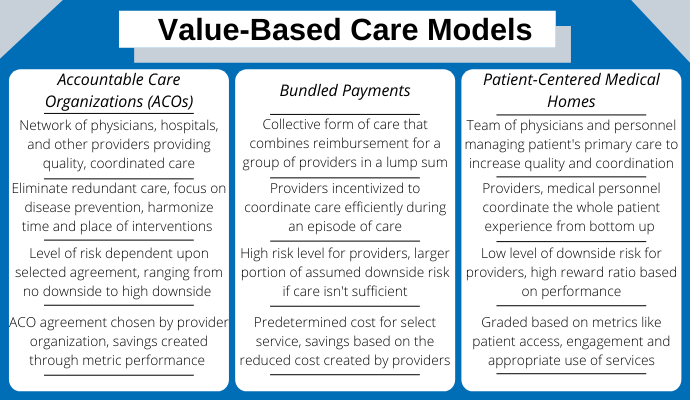
To participate in value-based care, CMS has developed several models for providers, such as the accountable care organization, bundled payments, and patient-centered medical homes.
WHAT VALUE-BASED CARE MODELS ARE AVAILABLE?
Source: Xtelligent Healthcare Media via Canva
Value-based care comes in a variety of types, generally differing as to the risks assumed by providers and sharing of savings or losses.
Accountable care organizations
An accountable care organization (ACO) is a network of physicians, hospitals, and other providers that give Medicare beneficiaries coordinated, high-quality care. CMS designed the program to help providers ensure that patients receive the most appropriate care at the right time. ACOs also aim to prevent unnecessary and redundant services while reducing medical errors.
Providers volunteer to participate in an ACO, such as the Medicare Shared Savings Program, Advance Payment ACO Model, or the Pioneer ACO Model. Under the payment model, the network of providers shares the savings if the ACO is able to deliver high-quality care and reduce healthcare costs.
On the other hand, providers in most ACOs must assume some financial risk for joining. While the potential of savings could be significant depending on the agreement, there is also a potential for shared losses. Providers may have to repay Medicare for not providing value-based care to patients.
“We see development of and participation in ACOs as an important part of our future as we move from a fee-for-service based payment system to population-based models based on quality, safety, and the patient experience,” said Lee Huskins, President and Chief Administrative Officer at John Muir Health’s Physician Network, to RevCycleIntelligence.com.
Bundled payments
A Bundled payment, or episode-based payment, is a single payment for services provided for an entire episode of care. Providers are collectively reimbursed for the expected costs to treat a specific condition that may include several physicians, settings of care, and procedures.
For example, CMS would combine the set payment to the hospital, surgeon, and anesthesiologist if a patient undergoes surgery, rather than paying each separately. Historical prices determine the bundled payment.
Value-based care is still a new concept for most healthcare providers, and many are still trying to implement the appropriate systems into their workflow.
The bundled payment relies on a certain level of risk. If providers can decrease the cost of the services below the bundled payment price, they can pocket the savings. However, if the costs are higher, providers bear a financial loss.
“Thus, bundled payment arrangements present many opportunities to re-tool the types and mix of post-acute care, and materially improve patient care and lower costs,” explained the American Hospital Association in a statement to the House Health Subcommittee of the Committee on Energy and Commerce. “Such efforts may include more standardized hospital discharge practices and post-hospitalization protocols for medical, rehabilitation and other post-acute care services.”
Patient-centered medical homes
The patient-centered medical home (PCMH) is a care delivery model that coordinates patient care through a primary care physician. The PCMH is designed to provide patients with a centralized care setting that manages the different needs of a patient.
The PCMH certification indicates that providers deliver patient-centered care, team-based methods, population health management, personal care management, care coordination, and consistent quality care. Patients in a PCMH can expect to develop unique, one-on-one relationships with their care providers, who determine healthcare needs based on medical and environmental factors.
Through this value-based care model, a Colorado-based PCMH reported a 15 percent decrease in emergency department visits, an 18 percent reduction in inpatient admissions, and a return on investment of $4.50 for every dollar spent. Another Maryland-based PCMH stated that it saved $98 million and increased its quality scores by 10 percent in one year.
HOW POPULAR ARE VALUE-BASED CARE MODELS?
In reality, value-based care is not an option for most healthcare providers. As HHS pushes to move more payments to alternative payment models, more providers feel pressure from public and private payers to participate in alternative payment models.
CMS has also expanded participation in value-based care programs, such as the MACRA rule and the Value Modifier program. For example, the MACRA rule applies to eligible clinicians, including ambulatory physicians, physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists. As the program matures, CMS intends to expand eligibility requirements to encompass more providers.
Eventually, CMS aims to tie all Medicare payments to value-based care models.
Several incentive programs have also helped providers quickly transition to more value-based care methods, such as the EHR Incentive Program. According to the Office of the National Coordinator for Health Information Technology, more than 90 percent of hospitals have certified EHR technology.
WHAT SUCCESSES HAS VALUE-BASED CARE ACHIEVED?
In 2015, HHS announced that 20 percent of Medicare payments were made through a value-based, alternative payment model. In the same announcement, HHS reported that ACO programs had saved $417 million for Medicare and value-based payment models helped reduce hospital readmissions in Medicare beneficiaries by eight percent.
Updated data from 2020 indicates savings have increased by 10 times since 2015 to a total value of $4.1 billion. Furthermore, the latest projections from CMS expect all Medicare payments to go through value-based models by 2030.
A CMS initiative that has quantified value-based care success is the Value Modifier program, which adjusts Medicare payments based on positive or negative quality assessments. In 2016, only 129 physician groups received an increase in Medicare payments of 15.92 percent or 31.84 percent.
The majority of physicians, representing 8,208 total, will not see any change in payment adjustment due to a neutral performance or insufficient data.
Value-based care is still a new concept for most healthcare providers, and many are still trying to implement the appropriate systems into their workflow.
“The transition from fee-for-service to pay-for-value has been referred to as one of the greatest financial challenges the U.S. healthcare system currently faces,” stated a survey from the Healthcare Information and Management Systems Society.
“Although this change is expected to happen over an extended period, CMS has announced aggressive goals for making the move with Medicare providers and hospitals. This requires healthcare providers to effectively navigate the challenges posed by a payment model that requires sharing and analyzing of data in ways that fee-for-service and its legacy revenue cycle management systems and business processes never contemplated.”
As new programs, such as MACRA emerge, and healthcare organizations become more comfortable with new tools, such as EHR systems, value-based care has the potential to decrease spending further and improve quality of care.
