Medical Billing Complexity Highest for Medicaid Fee-for-Service
Physicians faced up to $54 billion in challenged claim revenue in 2015, with Medicaid fee-for-service driving the bulk of medical billing complexity, a new study revealed.

Source: Thinkstock
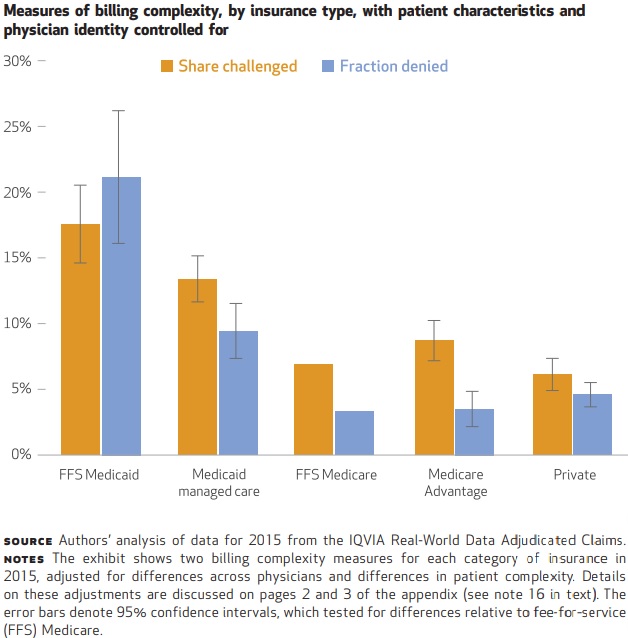
- Medical billing for Medicaid fee-for-service claims proved to be the most complex across all insurers. The public payer had a claims denial rate 17.8 percentage points greater than the rate for Medicare fee-for-service claims, a new Health Affairs study showed.
Based on the data of 68,000 physicians and 44.5 million claims from the IQVIA Real-World Data Adjudicated Claims database, lead author and Associate Professor at the Vancouver School of Economics, British Columbia Joshua D. Gottlieb found that Medicaid fee-for-service had the greatest medical billing complexity across all measures, not just claim denials rate.
Medicaid challenged 18 percent of fee-for-service claims in 2015 compared to just 6 percent of claims challenged by private payers, reported Gottlieb and his colleagues, Adam Hale Shapiro, Research Advisor at the Federal Reserve Bank of San Francisco and Abe Dunn, Assistant Chief Economist at the Bureau of Economic Analysis in the Department of Commerce.
The share of claims challenged for Medicaid fee-for-service was also 10.7 percentage points higher compared to Medicare fee-for-service.
Source: Health Affairs
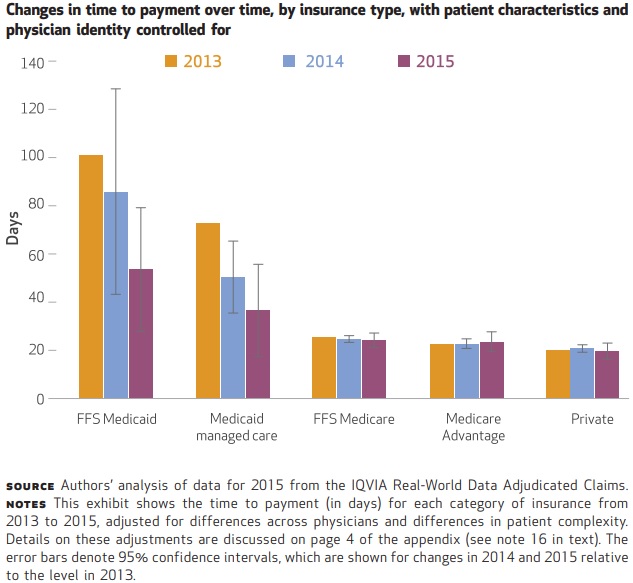
Additionally, Medicaid took 19 days longer to adjudicate claims for fee-for-service versus Medicare fee-for-service.
READ MORE: How to Maximize Revenue with Improved Claims Denials Management
Medicaid managed care had the second most complex medical billing process, researchers added. The claims denial rate was 6.1 percentage points above the rate for Medicare fee-for-service.
Medicare fee-for-service and private payers scored similarly on complexity measures, researchers added. Private payers were just 1.3 percentage points more likely to deny a claim compared to Medicare fee-for-service. But they paid claims 4.1 days faster.
“Although administrative costs are an essential input in overall healthcare production, the significantly lower complexity we observed for fee-for-service Medicare billing relative to fee-for-service Medicaid billing indicates that there may be ways for Medicaid to reduce its billing complexity and associated costs,” Gottlieb et al. wrote. “In turn, such reforms might increase physicians’ propensity to accept public insurance and use public healthcare resources more efficiently.”
Physicians may already hesitate to take on Medicaid patients because of the dramatic reimbursement shortfall. The American Hospital Association (AHA) recently reported that Medicaid reimbursement was $20 billion short of actual hospital costs in 2016, meaning Medicaid paid just 88 cents per dollar spent by hospitals to provide care to Medicaid patients.
Other recent research also shows that generating a profit on Medicaid admissions and care is tricky. A 2016 Health Affairs study uncovered that Medicaid hospital admissions can be profitable to safety-net hospitals, but only if the organizations receive supplemental reimbursement, such as Disproportionate Share Hospital payments.
READ MORE: The Difference Between Medicare and Medicaid Reimbursement
Another 2016 study in the same journal also showed that state taxes and other fees that help to finance the Medicaid program decreased Medicaid reimbursement by 11 percent for disproportionate share hospitals.
The question of profitability coupled with medical billing complexity could drive more providers to stop accepting Medicaid patients, Gottlieb et al. explained.
While Medicaid was the worst offender in the study, physicians still faced significant administrative burden and costs associated with medical billing across insurers, the researchers added. Payers challenged up to $54 billion in claims in 2015, the data revealed.
“To interpret this number, note that physicians might be able to recover some of these challenged payments by hiring additional personnel or upgrading billing technology,” the study stated. “Presumably they would attempt to do this if it were worthwhile. Therefore, the administrative costs are likely to exceed the potential revenue, and our estimated amount challenged provides a strong indication that the administrative costs are very large.”
However, there is hope for reducing medical billing complexity.
READ MORE: Medicaid Acceptance, Payment Rates Both on the Decline
Medicaid fee-for-service may be the most complex, but the program has improved over time. For example, the time to payment for Medicaid fee-for-service claims fell from 101.2 days in 2013 to 53.6 days in 2015.
Medicaid managed care also dropped from 72.7 days to 36.6 days in the same period. In addition, Medicaid managed care’s share of claims challenged declined, falling from 26.2 percent in 2013 to 20 percent in 2015. The claims denial rate also dropped from 17.1 percent to 8.9 percent in the same period.
Source: Health Affairs
Researchers also observed improvements across other insurers. Notably, private payers reported a slight decline in claims denial rates, from 5.6 percent to 3.9 percent between 2013 and 2015.
Medicare Advantage denial rates dropped by a similar amount, from 4.2 percent to 3 percent.
Claim denial rates for Medicare fee-for-service remained relatively the same across the three-year period.
Public and private payers should continue to decrease medical billing complexity to realize patient care benefits, Gottlieb et al. advised.
“When billing complexity declines, both physicians and patients stand to benefit,” they wrote. “Time that physicians don’t spend on administration could instead be used to treat more patients or extend the length of visits, ultimately increasing the productivity of physician care. Easier billing processes reduce staffing needs and billing expenses, which could raise physicians’ incomes or free up resources for patient care.”
