Quality Payment Program Top Regulatory Burden for Practices
Medical practice leaders were particularly dissatisfied with the Quality Payment Program’s reporting requirements, scoring method, feedback, and lack of measures.
Source: Thinkstock
- For the second year in a row, medical practice leaders said the Quality Payment Program was their top regulatory burden in 2018.
Eighty-percent of the 426 group practice leaders recently surveyed by the Medical Group Management Association (MGMA) cited the Quality Payment Program and its two payment tracks – the Merit-Based Incentive Payment System (MIPS) and Advanced Alternative Payment Model (Advanced APM) pathway – as either very or extremely burdensome.
About 82 percent of medical practice leaders in the previous year’s survey also said the Quality Payment Program, along with MIPS and Advanced APMs, were a significant burden on their practice in 2017.
MACRA’s Quality Payment Program again beat out prior authorizations (82 percent), lack of EHR interoperability (80 percent) and government EHR requirements (77 percent) as the top regulatory burdens of 2018.
“This precipitous increase in regulatory burden over the past 12 months should alarm policymakers,” Anders Gilberg, MGMA’s Senior Vice President of Federal Affairs, stated in an emailed press release. “MGMA's survey provides valuable insight into what’s ailing medical practices. Its findings will enable HHS to refocus and redouble its efforts to create meaningful regulatory relief for physician practices.”
READ MORE: How Can CMS Improve MACRA’s Quality Payment Program, MIPS?
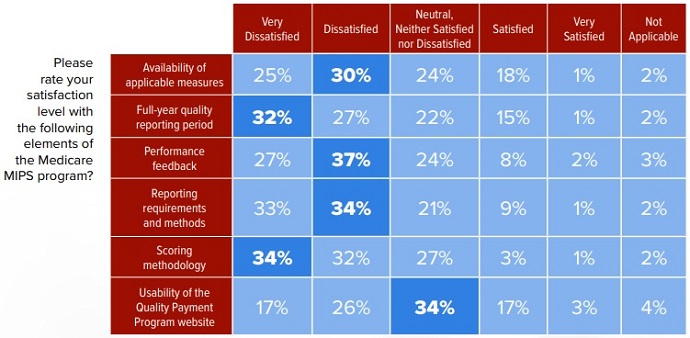
Medical practice leaders were most dissatisfied with the Quality Payment Program’s reporting requirements. Approximately 67 percent of respondents said they were dissatisfied with the value-based purchasing program’s MIPS reporting requirements and methods.
Only 10 percent of survey participants reported feeling satisfied with how their practice must report data to MIPS.
Source: MGMA
Respondents particularly took issue with the full-year reporting period for the quality performance category of MIPS. About 59 percent of group practice leaders said they were dissatisfied or very dissatisfied with the 365-day period.
CMS significantly upped the quality performance category reporting period in 2018. For the first Quality Payment Program performance year in 2017, eligible clinicians only had to collect data on at least one measure for one patient for one day.
The federal agency offered the reduced quality reporting period in 2017 to give eligible clinicians an opportunity to get used to the new program.
READ MORE: Key Ways to Succeed Under MACRA’s Quality Payment Program
In addition to Quality Payment Program reporting, medical group leaders were also dissatisfied with the program’s scoring methodology (66 percent), performance feedback (64 percent), and availability of applicable measures (55 percent).
Additionally, medical practice leaders specifically felt the Quality Payment Program’s MIPS was a burden for their organization.
Nearly 78 percent of respondents reported participating in MIPS in 2018. However, the majority of respondents also reported that the Medicare value-based purchasing program does not align with their practice’s priorities.
Sixty-seven percent of group practice leaders felt MIPS, as implemented by CMS, does not support their practice’s clinical quality focuses. Just 24 percent of respondents said the value-based purchasing currently supports their quality priorities.
Respondents also expressed confusion over how MIPS works. Over one-half of medical practice leaders (51 percent) reported a lack of understanding among their clinicians on how MIPS evaluates them on quality.
READ MORE: Impact of Quality Payment Program on Medicare Reimbursement
Another 49 percent of survey participants also stated that their clinicians do not understand how the Quality Payment Program track assesses them on healthcare costs and utilization.
A significant portion of medical practices would participate in the Quality Payment Program’s Advanced APM track instead of MIPS. However, the survey revealed that practices do not have many Advanced APM options.
Forty-four percent of respondents said their group practice is interested in joining an Advanced APM as long as the model is clinically relevant and aligned with their goals. Only 22 percent reported disinterest.
But over one-half of survey participants (55 percent) said Medicare currently does not offer an Advanced APM that is clinically relevant to their practice.
Medical practice dissatisfaction with the Quality Payment Program may be impacting the general transition to value-based reimbursement.
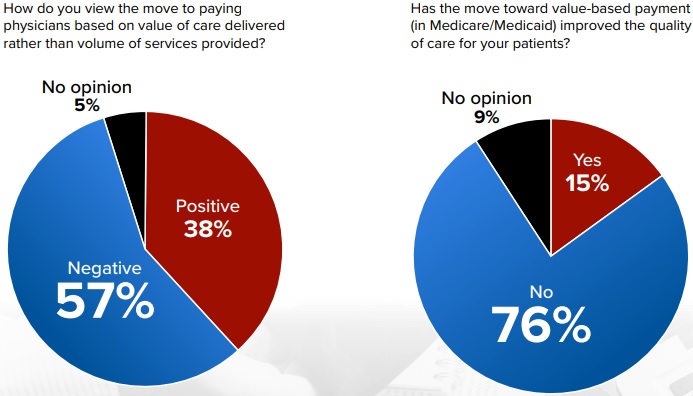
Fifty-seven percent of group practice respondents stated that the move to value-based care was negative, and another 76 percent said the moved to value-based reimbursement in Medicare and Medicaid has not improved care quality.
Source: MGMA
Almost all group practice leaders (90 percent) reported that the value-based reimbursement transition in Medicare and Medicaid has increased the regulatory burden on their practice.
Negative views on the move to value impacted the success of value-based reimbursement, the survey showed. Just eight percent of survey participants said the move to value-based payment has been successful to date, and 79 percent said the move has been unsuccessful.
Thirteen percent of respondents had no opinion on the transition’s success.
Reducing the regulatory burden of value-based reimbursement programs may be the key to pushing more group practices to make the move away from volume. Policymakers should consider the burden required initiatives, like the Quality Payment Program, have on providers and whether modifying reporting requirements and applicability of measures would promote greater participation in the move away from fee-for-service.
