Real Costs Up to 8% Higher for Some Cancers in Oncology Care Model
Actual costs for eight cancer types in the Oncology Care Model were significantly higher than predicted costs, spelling trouble for some providers in the bundled payments model.

Source: Thinkstock
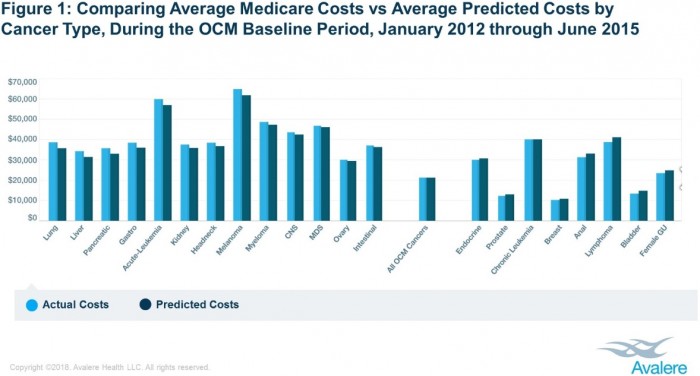
- New research shows actual episode costs for certain cancers covered by Medicare’s Oncology Care Model differed by as much as eight percent, on average, from the predicted costs per episode.
The Oncology Care Model (OCM) is a voluntary bundled payments initiative that aims to decrease costs and improve care quality for cancer care. The five-year model currently has 179 oncology practices and 13 payers participating across the country.
The OCM includes bundled payment tracks for 21 cancer types, including cancers impacting the breasts, prostate, lungs, and intestines.
However, a new analysis from healthcare consulting firm Avalere showed that providers who treat certain types of cancer may perform better under the OCM.
Using Medicare Parts A and B fee-for-service claims and Part D prescription drug event (PDE) data under a CMS research data use agreement, researchers found that eight cancer types in the bundled payments model had actual costs significantly higher than the predicted episode costs. Actual spending exceeded the estimated costs by three percent or more.
Notably, lung and liver cancer episodes had actual costs eight percent higher, on average, than predicted costs.
In total, the eight cancer types represented 10 percent of all OCM episodes.
Exceeding the estimated episode costs results in a financial loss for providers in the OCM. And providers in the two-sided financial risk track of the bundled payments model must repay CMS a portion of the shared losses.
Source: Avalere
On the other hand, other cancer types in the OCM had average actual costs below the predicted episode costs. Five cancer types had actual episode costs that, on average, fell below the estimated costs by three percent or more.
Bladder and female genitourinary cancers other than ovarian generated significantly lower actual costs. Episode spending for these cancer types were five percent lower than predicted costs.
Together, the five cancer types accounted for almost one-half of all OCM episodes.
However, researchers noted that breast cancer was among the five cancer types with actual costs below predicted expenditures. Breast cancer episodes were very common in the OCM, accounting for 38 percent of the episodes studied.
Taking away breast cancer, the four other cancer types with real costs under the predicted costs represented just 11 percent of OCM episodes.
The remaining 41 percent of OCM episodes involved eight cancer types that had average actual costs within negative and positive three percent of predicted costs.
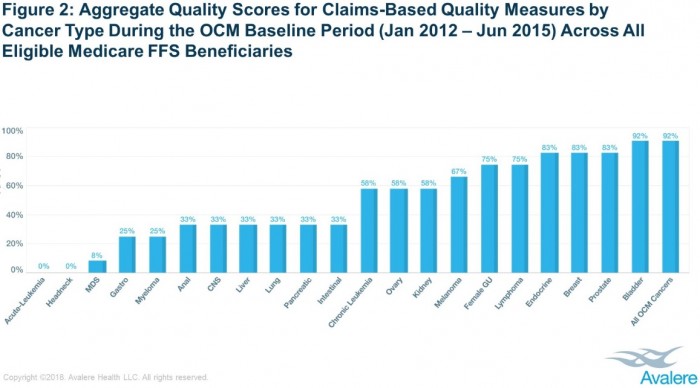
Additionally, the Avalere analysis showed that provider performance on claims-based quality measures also significantly varied by cancer type.
The OCM ties a provider’s performance-based payment to how they perform on 12 quality measures, three of which are claims-based.
Using the claims-based measures, researchers found that aggregate quality scores were lower for some types of cancers. For example, providers earned none of the possible quality points for acute leukemia and head-and-neck cancers, on average.
However, providers achieved 92 percent of the possible quality points, on average, for bladder cancers.
Source: Avalere
In total, eleven cancer types achieved less than 50 percent of the possible quality points. The cancers accounted for 20 percent of all OCM episodes.
The remaining ten cancer types in the bundled payments model achieved, on average, over 50 percent of the possible quality points. The cancers represented 80 percent of OCM episodes.
For the majority of cancer types with high actual-to-predicted cost ratios, the cancers also had low aggregate claims-based quality scores, researchers pointed out. Similarly, the bulk of cancer types with low actual-to-predicted cost ratios also had high claims-based quality scores.
“Cancer episodes for which actual costs are greater than predicted costs and for which quality scores are low will adversely affect a participant’s ability to earn performance-based payments,” stated Matt Brow, President of Avalere. “Identifying these types of challenges are essential to ensuring the Oncology Care Model succeeds in rewarding efficient and high-quality care.”
Developing strategies to account for differences in the predicted cost and actual cost of cancer treatment will also be key to ensuring patient selection is “neither a successful nor necessary strategy for OCM participants to earn performance-based payments,” researchers concluded.
